Andrea's blog
Double Mastectomy: 2 Weeks Post-Op
Week 1 was a physical struggle.
Week 2 was definitely more mental and emotional, with some slow physical progress. About day eleven post-op, I started trying to make some efforts toward feeling more normal. I put on (stretchy, soft) jeans instead of sweats. I wore dangly earrings. I spent more of the day downstairs than in my bed or in the recliner in our bedroom. I rode in the car with Ben to pick Paxton up from school at the edge of our neighborhood (which was the first time I even left the house!) I even put on a TINY bit of makeup--which is how I realized my eyebrows and eyelashes have thinned again.

That seems to be the pattern about 4-6 weeks after chemo ends, but since I didn't lose my hair during Taxol, I wasn't expecting to lose my eyebrows and eyelashes again. I took that kind of hard. They'll grow back quickly and plenty thick on their own, but let's be clear, I did NOT need another reason to be frustrated with my reflection -- or to see 1,000 ads for lash boosting serums, magic mascara, magnetic eyelashes, etc. which honestly just makes me feel worse about them -- BACK THE FRICK OFF Facebook!
Otherwise, I continued to take it very easy. Lots of rest. My biggest activity in each day was taking a shower and getting dressed, and then changing clothes again that night for bed. That's it. That was the only physical goal--and it was plenty, considering how slow and methodical I had to be to do those tasks.
I started to notice my arm and shoulder mobility improving. While I still am not able to move quickly or hold/push/pull anything heavier than a couple of pounds, I have a little better range of motion before it starts to pull on my incisions or become uncomfortable. So, that's encouraging. I also found that I can wear normal shirts (not just button-downs) as long as they are stretchy enough, which makes me glad I didn't buy a bunch of special clothes for post-surgery. But I am still sporting a fanny pack or an apron to hold my drains, which are extremely annoying.
When I found out I didn't have to wear that awful compression bra after week 1, I tried a couple of days with no bra at all, thinking that would be great, and found that it was just as awkward and uncomfortable. Although I wasn't wearing a bra, the under-my-skin tissue expanders and the surgical tape all still made me feel like I was wearing an iron bra that was too tight, without anything on at all, which was very disorienting. I found that wearing a soft cotton bra was much more "normal" feeling. At least then that wearing-a-bra feeling made sense.
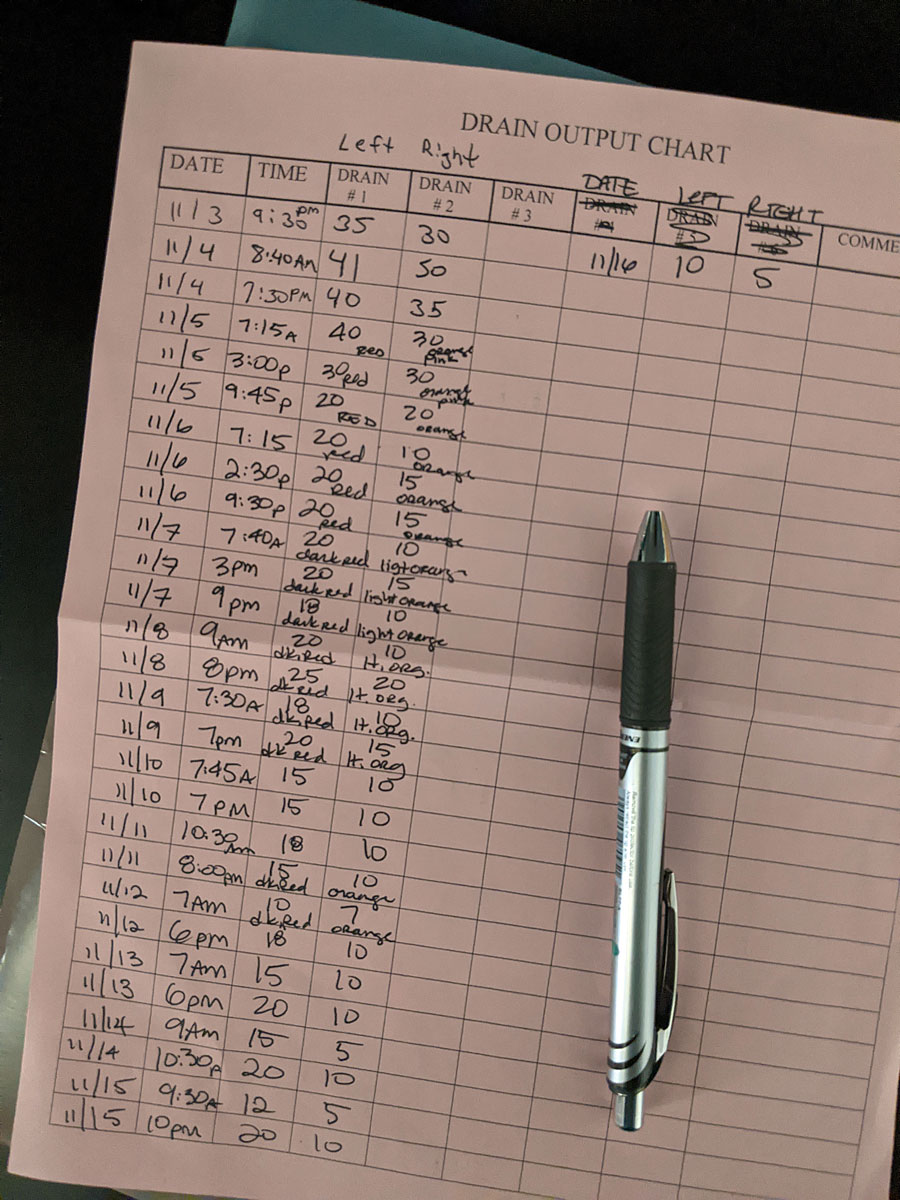
In the meantime, I continued to monitor the output on those drains in the hopes that I could have them both removed at my 2 week post-op appointment. One seemed to be slowing down and changing colors as it should. The other stayed stubbornly about the same, but slightly less each day. The goal is less than 30ml per 24 hours.
Today, was my 2 week post-op appointment with my plastic surgeon (well, technically with his nurse). I was instructed to take the tape off of all the incisions this morning in the shower, which was a fairly nerve-wrecking exercise. You certainly don't want to "rip the bandaid off" in this moment. I took my time, but without a mirror, and without knowing what I'd find underneath the gauze, each pull of tape felt like tiny scary torture. It both hurt (any tape that stays put for two weeks through daily showers is pretty strong) and was terrifying to wonder what was beneath the tape. I did it though, and the incision scars (aka battle scars) aren't too terrible or Frankenstein-y. I think (hope) they'll fade over time. At the moment, it doesn't really matter what they do (as long as they heal), because they'll cut them back open again when I have my exchange surgery in a few months.
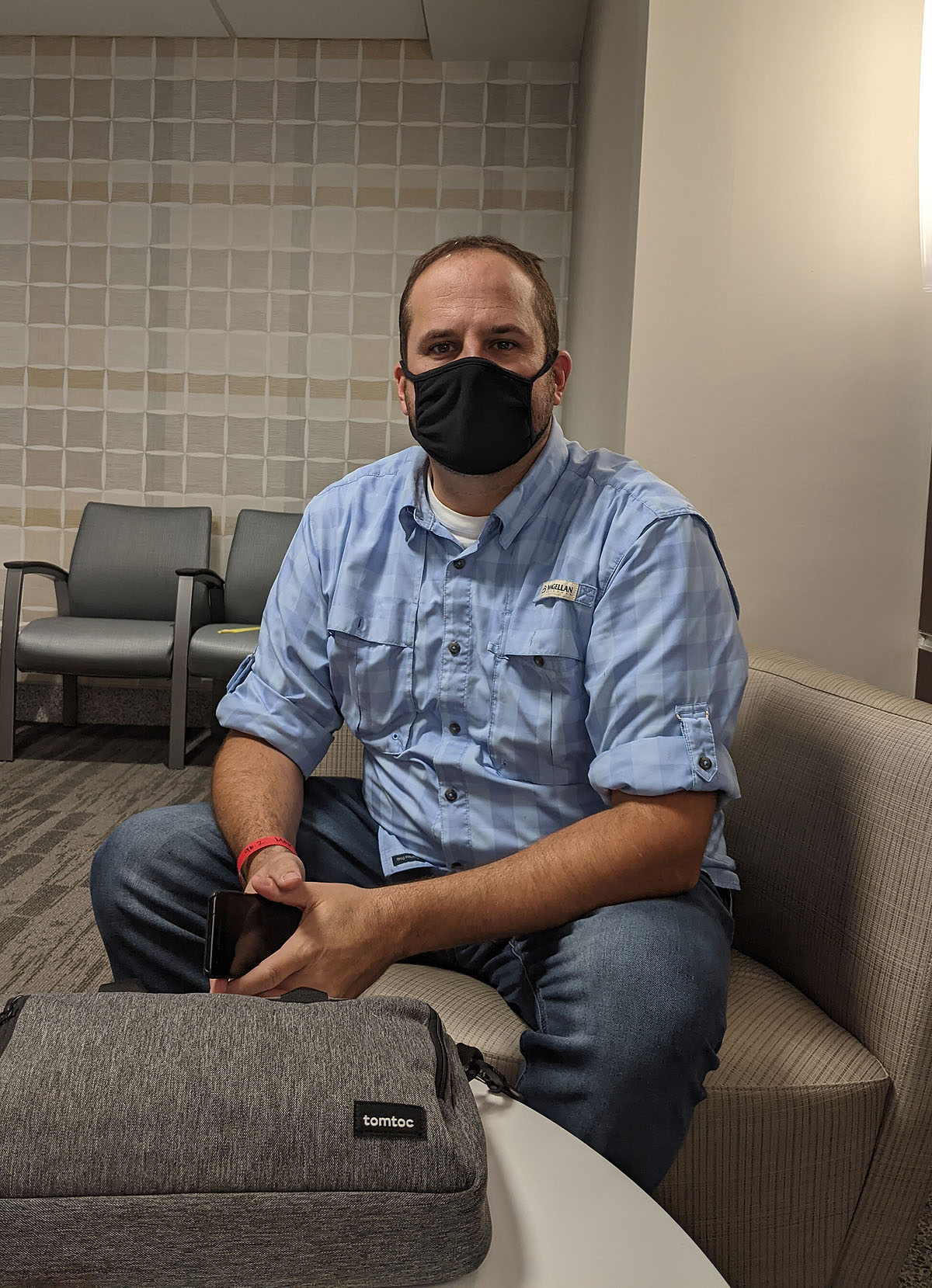
I had a LOT of anxiety going into this appointment. I had no idea if I would get my drains out, if everything looked like it should, if I had been healing properly, if I had been moving enough and making enough physical progress, if I'd get a "fill" or saline replacement of the air pumped inside those expanders, if any of it would hurt, if I'd be given permission to start walking or exercising, etc. etc. Also, I hadn't left the house in two weeks (well, neighborhood, technically, since I did take that one little joy-ride to the edge of the neighborhood on day 11). Isolation does something nasty to a person's mental state--it's fear and anxiety inducing, especially in the middle of a pandemic. Ben drove me to my appointment and did his best to calm me down without dismissing my anxiety. I'm not sure I really calmed down until hours afterward though.
The appointment was quick. The nurse checked out my incisions, looked at my drain log, decided to remove one drain, told me I could definitely start walking (and that it might help progress the other drain along), and sent me on my way with a new appointment for Friday to (fingers crossed) take out that other drain. Taking the drain out was not a big deal and did not hurt. That doesn't mean I wasn't extremely nervous about it. Next time, I'll be much more calm. Essentially, she cut the suture, which was slightly uncomfortable, but not painful, and told me to take a deep breath. While I was breathing out, she pulled all of the drain tubing out and I didn't feel anything remarkable. It was over fast. I did NOT look, and in fact, I told Ben to move to another chair so I could look at him and not be able to see myself or the nurse in the mirror next to him. He said (with a grimace and a shudder) that it looked like a very long tapeworm that she pulled and pulled and pulled out. I think I'm glad I didn't watch.
So that's it. Now I'm home and gearing up to walk a lap or two up at the park behind our house. I know the "ok" to walk and get a little exercise and fresh air will help my mood, and probably restore some energy and life back into me.
We'll try again on Friday to see if my other drain is ready to come out. If it is, I'll be able to start the switch over from air-filled to saline as early as next Monday. If it's not...we just keep waiting. While most don't, some people have their drains for up to 6-8 weeks! I'm hopeful that won't be me, but trying not to set any expectations. In the meantime, I'm going to start trying to add back some regular activities to my day to relieve Ben--like making coffee and washing dishes, paying a little better attention to what the kids are (or aren't) doing, and hopefully driving (at least in the neighborhood).
This is a slowwwww process to get back to "normal". I'm trying to stay patient and positive and be accepting of a much much slower pace and output than I am accustomed to. The doctors say around 4 weeks most people feel like they turn a corner. Some who have gone through it say it takes 6-8 weeks. Some say their energy levels don't come back for months. I'll keep you posted...

Pause for Thought
The first few days after my surgery were kind of a sweet relief. No work. No need to be attached to my phone. No reason to feel guilty about not being productive. I could wear sweats and not put on makeup and sleep all day if I wanted to (and I did).
I've had a stressful year. I deserved a break and some rest.
But here's the thing I was warned about, but didn't pay enough attention to -- As soon as there was a true pause, then it ALL caught up to me. And there was nothing around to distract me from the gut punch and pain of each and every thing that has been stolen from me this year.

Perhaps this is all a little overly dramatic--but allow me a (few) moment(s) of wallowing, will you?
Suddenly I am in physical pain with limited mobility from a glorified amputation that I didn't want. I have foreign objects implanted under my skin that make me feel like a cyborg. I look in the mirror and I have a super-short, very gray haircut with thinning eyebrows and eyelashes, that ages me at least 10 years and isn't the "me" I recognize (although it probably matches the way I feel this week).
And that's just the physical.
Working from home and being self-employed is both a blessing and a curse. Yes, I have the flexibility to do my job and have kids at home all day, and have cancer treatments, and take care of my mom in the hospital, and be in Chicago with my family when my dad passed away. But what have the costs been? I had to quit a job that I loved to devote my time and mental and physical energy to cancer treatments. I largely ignored my kids and husband and sacrificed time spent with friends to use the energy I do have to push myself to work and try and earn as much of an income as I'm able in the midst of one tragedy and setback after another. Or, I had to shut down my business completely for weeks or months at a time to drop everything and tend to my own health, my father's death or my mom's health.
Everything COVID is infuriating and infiltrating every aspect of our lives in this already difficult year, making everything that used to be uplifting and fun and regulating and grounding, now a depressing struggle. We have not had a "normal" week since March (nor has anyone, I'm aware). Everything that used to be a go-to pick-me-up has been poisoned with mask requirements and social distancing and fear-inducing restrictions. Instead of feeling refreshed and uplifted and grounded by things like shopping and hanging out with friends, and going to church or school, or traveling and concerts and sporting events--all of those things have been poisoned with the stamp of COVID. Some of them we can still do, but that COVID stamp just puts a bitter taste all over everything, leaving me sad and more depressed, not uplifted and encouraged.
And then there's the cancer factor. My treatment has been successful, and that's good. But potential recurrence will hang over my head forever. It will be a filter over everything in my life moving forward, whether it ever returns or not. Unfortunately, recovering from surgery isn't the "last step" -- not for us anyway. Other people will move on (and they should), but Ben and I and the kids will be forever changed and affected by the trauma of this year. There are too many stories of people we know well who had great and promising results from their cancer treatments, but then a few short months or years later, it took their life.
It's no wonder we're exhausted and feel defeated.
I've been told I have a hard time expressing (or even acknowledging) my feelings. For me, it's easier and "more efficient" to shrug things off, let things go, focus on the positive, and do what I CAN instead of brooding about what I can't. But when everything stopped in the past two weeks, and I had time to sit and reflect on all that has happened this year, the feelings I normally refuse to allow began crawling their way up to the surface. So, I'm acknowledging them and expressing them while they are making themselves known.
I'm angry that I have to go through any of this.
I'm discouraged that there never seems to be an ending.
I'm scared that the cancer will come back and I won't be prepared for it.
I'm annoyed when my double mastectomy and reconstruction is compared to a breast augmentation.
I'm grieving that I can't call my dad anymore.
I'm worried that irrepairable damage has been done to some of my relationships.
I'm mourning the loss of my youth and innocence (or perhaps more accurately, ignorance).
I'm frustrated at the reflection I see in the mirror.
I'm resentful toward all of the things that took time away from me when I felt good this year.
I feel inadequate as a parent with no real way to help my kids navigate through all the worry and disappointment from this year.
I'm resigned to constant disappointment.
Honestly, I'm not sure I know what to DO with any of these feelings, other than trying to be transparent and authentic as I record this journey and process. It's uncomfortable for me, and feels like complaining and whining about things that can't be changed, which feels pointless and wasteful. Truthfully, my instinct is to ignore them and look at the bright side, be positive, and press forward--and most days I will. The past week though, I've been grumpy and depressed and self-loathing and wallowing, and I wanted to be honest about why.
Double Mastectomy: Week 1 Recovery
What does the first week of recovery after a bilateral mastectomy with tissue expander reconstruction look like? I'd like to think it looks like this:

But the truth is, it looks more like this -- sleeping or laying as still as possible, switching between a propped up pillow on the bed or a borrowed recliner (which has been a lifesaver), trying to stay comfortable, with all my necessities in a small circle around me, within my t-rex arms reach:

Ben has found joy in taking pictures of me sleeping, and it seems I strongly resemble an old man while I sleep. I guess I can laugh about it...but I sure am feeling frumpy and uncomfortable.

You would think I'd have gotten bored doing nothing this week, but to be honest, I've absolutely needed to do nothing, have nothing expected of me, and not try to think about anything remotely complicated. Most of my energy is going into remembering when to take which medicine, focusing on not scratching where the tape is irritating my skin, and trying not to yank my surgical drains out by accident.
It's all tolerable, and only mildly painful, but recovery is definitely uncomfortable and all-consuming, at least so far. There's just no real relief from any of it.
I'm having to be selective about what I share here about this part of the process. I want to be open and descriptive about the realities of all of this, especially for anyone looking for a first-hand experience of something they'll have to go through themselves. But at the same time, my family and friends are reading this too, so I'm not really comfortable just baring everything. So, I'll do the best I can to describe what's going on and share a few PG-rated photos as I'm able.
Not the accessories I was hoping for...
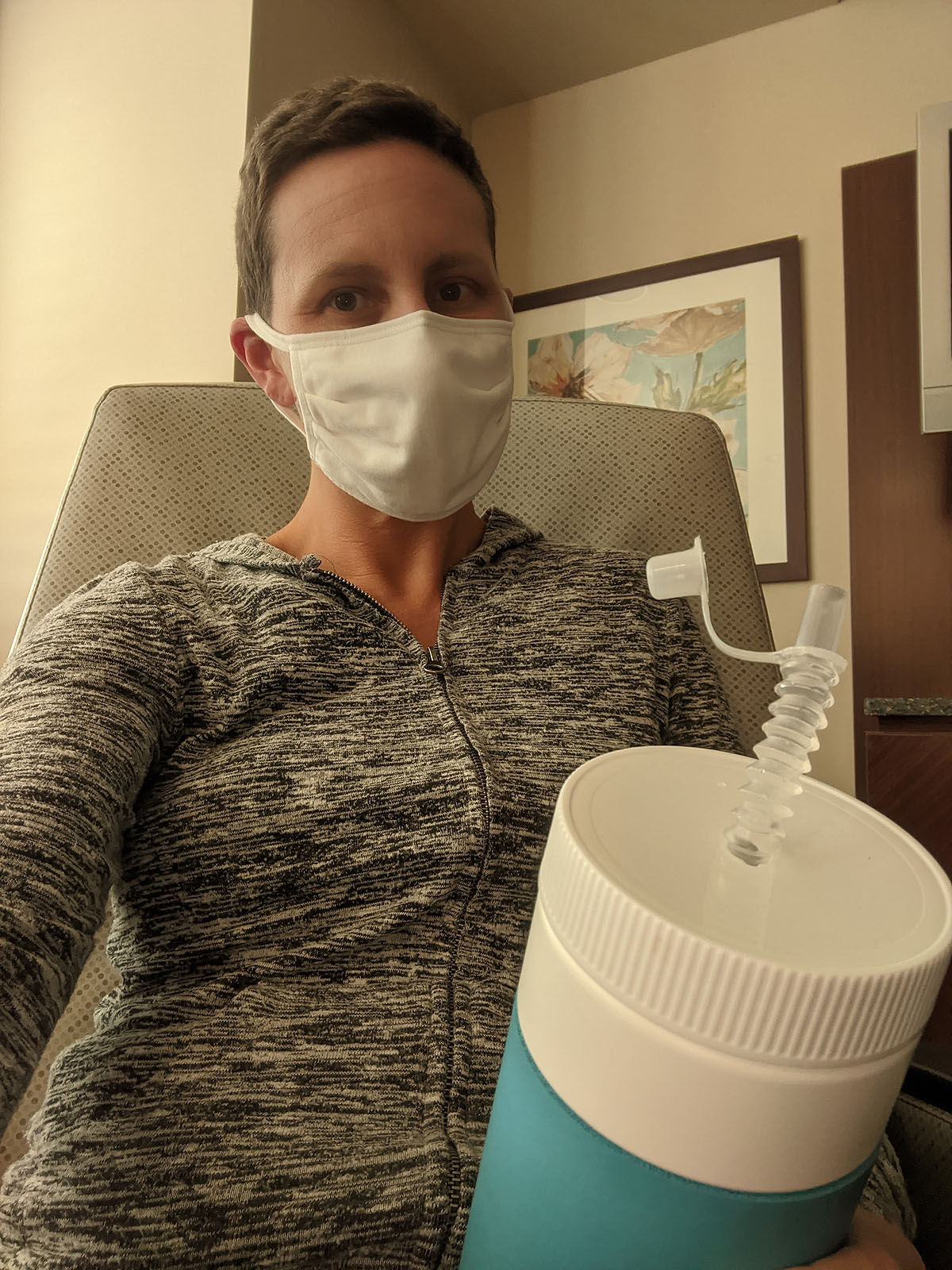
They sent me home from the hospital in this lovely get-up -- a compression surgical vest with two surgical drains, one on each side.

The vest is stiff and itchy and squeezes everything, which is already being squeezed and pulled together by clear tape across my entire chest, covering my incisions. Although it's yellow and bruised all across my chest, I don't have any pain from the long incisions on the sides of my breasts. Most of that area is numb from all the nerves being severed when all the breast tissue was removed. Although, I do have some random spots on both breasts where I still have feeling and sensation, where it is definitely tender. My understanding is that is normal, and may or may not ever improve. So, the fact that I have a few spots of working nerve endings was better than the complete numbness I was expecting.
But I can definitely feel pain where the lower band of the surgical vest presses into the open wounds where my drain tubes are sutured into my skin, and that has been the most painful part of this so far.
As far as pain relief, I took the narcotic pain pills they gave me for several days on a regular basis after I got home, which I'm sure helped me stay asleep and still. But by Friday (4 days post surgery), I decided to switch to alternating between tylenol and advil because the constipation that those narcotics causes was WAY worse than the pain! Once I got that under control, I was able to add a pain pill and muscle relaxer a day into the rotation, which I typically want late in the evening when I just haven't had any relief from the pain all day and need to fall asleep.
It was my understanding that I am supposed to wear this surgical vest until my 2-week follow up doctor's appointment. This morning, after a week of wearing it day and night, I called to be sure that was the instruction, and thank goodness, they said I don't have to wear it, because the tape is holding everything in place. That ought to bring me a lot of pain relief over the next week, and I wish I had listened better in the hospital to the instructions so I could have taken it off earlier! But, in my drug induced state, I remember my breast surgeon telling me to wear it all of the time, and the plastic surgeon telling me to wear whatever felt comfortable, so I had erred on the stricter side, to be sure.
Bruised & Battered

After a couple of days, my body started showing evidence of being bruised and battered from the surgery. This purple bruise under my arm is the nastiest looking one, and I think it might have been caused by the surgical bra rubbing and pressing against it in the hospital. Of course, I guess it's possible in surgery they had me harnessed up from that spot, to get access to all they were removing. In any case, it looks worse than it feels, thankfully. But it's definitely tender.

I also have a big section of bruising on my left side. I'm not really sure what part of the procedure would have caused that. It's slightly tender, but also looks worse than it feels.
What hurts the most are those tiny little drain tube incisions.
Drains, Drains, Go Away
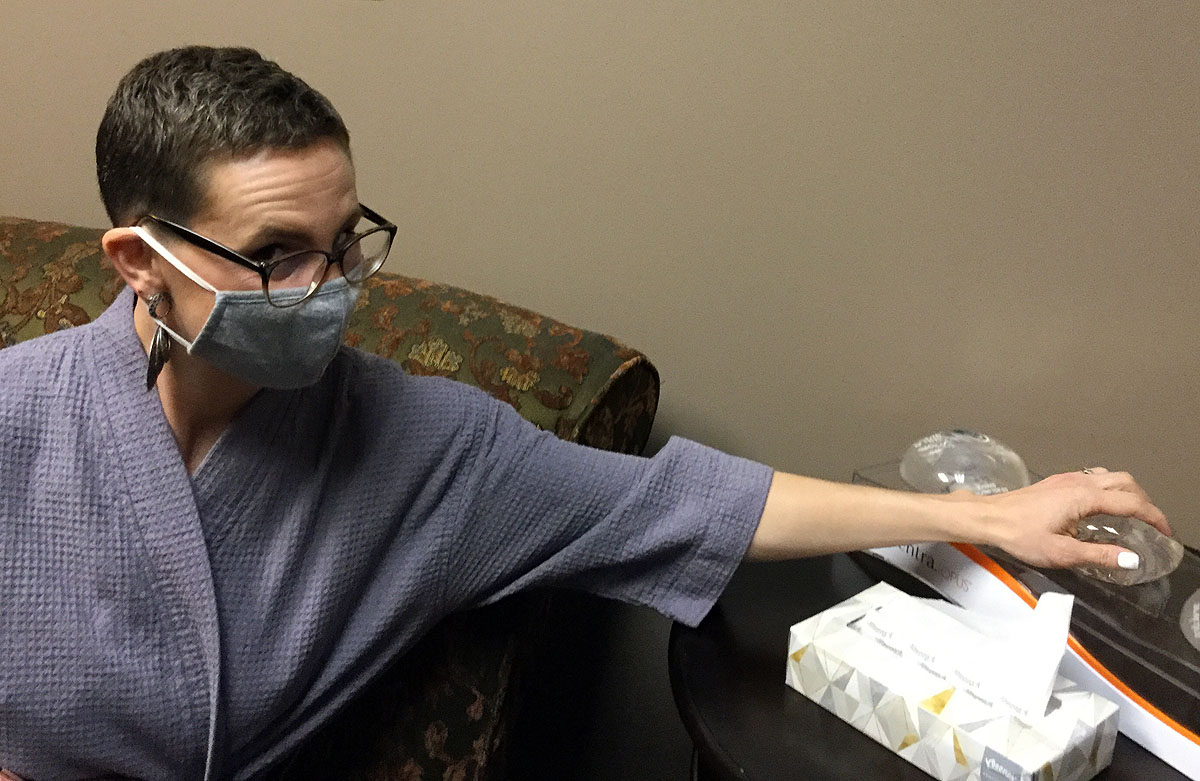
So let's talk about the drains. The sutures are itchy and bruised and painful, especially with a compression bra pressing on them 24/7. Taking off that compression bra should help with that. But carrying around two lumpy drains isn't a picnic either. They have clips that can hook onto the insides of a shirt, and my friends bought me a mastectomy robe that has pockets on the inside of it to hold the drains away from my skin, which works pretty well. I have to hook them both to a lanyard around my neck to take a shower so that they don't hang down and pull on the sutures. But, outside of the shower, I've found that wearing a waist apron with pockets or a fanny pack has been the best way to keep them lower by my hips and out of the way. Otherwise they create extremely awkward lumps inside my shirt. Also, there's nothing weirder than wearing a fanny pack to bed.

Two or three times a day, I have to strip the drains (squeeze fluid out of the tubes) and empty them into measuring cups to record how much fluid is coming out of each drain. Over time, the amount will decrease and the color of the fluid may change colors. While that initially sounded like a very scary and gross process, it's really not a big deal, and the amount of fluid has been slowly decreasing each day. My hope is that by my 2 week appointment, both drains will have slowed down enough that I'll be able to have them both removed at my appointment. And when I think about all that fluid collecting inside my body, I'm very thankful to have an easy way to get it out of my body!
New Foobs, Who Dis?
So, about my reconstructed breasts -- they actually look relatively normal right now (thanks to a nipple and skin sparing surgery option), but they feel very weird. They are filled with air, so they feel like overly inflated rubber balls, not squishy at all. I believe when I go to see the plastic surgeon, they will remove the air and refill them with saline, which I imagine will be a little softer and probably heavier. Even without a compression bra on, it feels like I'm wearing a very tight bra that I can't take off. Maybe some of that is the tape, but I've heard that feeling of tightness and pressure on your chest doesn't really go away.
Because they look "acceptable", I'm not dealing with much emotional trauma of them being removed, and I'm thankful for that. But, I haven't really seen the incision scars yet, and still have a long way to go before they are "done" (maybe by my birthday in April?).
Moving (or more accurately NOT moving) On...
One of the hardest things for me, is being still and not moving my body. I'm not supposed to reach my elbows above my head at all. I am not supposed to carry, push or pull anything more than 10lbs. It helps that I'm tall, so that I can stand on my tip-toes and use t-rex arms to reach for things like a plate in the kitchen cabinet or the microwave door, but I've had to be creative or ask for help in many other situations.
Getting dressed is a slow and tedious process, and trying to figure out what will be comfortable, whether I can get it on and off without raising my arms up too high, and then seeing how my lovely apron/fanny pack situation works with everything takes a good amount of my time each day. And let's just say, I'm not going to win any fashion awards this week. I've mostly looked like a clown. Leggings with an oversized stretchy t-shirt and a zip-up hoodie seem to work best.
Such limited movement is a big change for me, and it's made the rest of my body feel pretty stiff and sore too. I'm used to running and twisting and jumping and reaching and moving my body in all kinds of crazy ways, so a week of immobility is definitely taking it's toll.
I'm doing my arm and shoulder physical therapy exercises, walking around the house and up and down stairs, but that's pretty much it. I'll be so thankful when I can really stretch and warm up my muscles and joints again.
Pathology Report
Briefly, because I don't have any specific details yet, my surgeon's secretary called me this week with a very general pathology report info. She wrote "benign" on the right side (non-cancerous side) and "Great!" on the report as a whole.
I have an appointment to see her on November 18th, where I expect to get more detailed information, but ultimately, we all assume that "Great!" means everything looked good, she got clear margins after removing all the breast tissue, and there isn't any additional cancer to treat at this point because all of it was removed or already killed by chemo. It sounds like my treatment has been successful!
So, that's what week 1 of recovery looks like for me. I'm trying to stay patient, stay still, and stay positive and am watching a lot of stupid television and catching up on my blogging while I am chair-bound. I expect the next week to be more of the same until I can get these drains removed.
And in the meantime, my whole family is enjoying the food that our friends from church have been bringing all week! It's been such a relief for Ben to not have to think about meals in addition to all the other things he's had to take over with me out of commission. So we are extremely thankful for that!
Double Mastectomy: Surgery Day
So many pills. I recieved my pre-surgery packet from the plastic surgeon's office and it included several new prescriptions -- pain killer, muscle relaxer, antibiotic and sleep aid. Plus all the regular pills I already take - antithyroid, multi-vitamin, probiotic, claritin, and biotin. It's going to take quite a spreadsheet to keep all these in order after my surgery. I tried to label them all so in case I was out of it, Ben would know what each thing was for and when I should take it!

Other pre-surgery to-do items were to get my Covid test (which came back negative), and get my nails done. Some friends had given me a gift certificate to a new salon and I decided to go ahead and get a dipped manicure and a pedicure right before surgery so that when I felt ugly and sore and beat up after surgery, at least I'd have pretty hands to look at.
Later, I heard some talk and warnings about not being able to have nail polish on when you go in for surgery, but it wasn't in my pre-op info, so I decided forgiveness was easier than permission. And having my nails done was really important to me. I don't know why I got stuck on that, but I might have fought someone if they told me I had to take it off. When you have no hair, can't wear normal clothes, or put on makeup or wear jewelry, and feel completely awful, I just needed something to feel like it looked pretty. And since it's a dip manicure, it should last me the full two weeks post surgery when I'm least able to do my own nails.

Somehow, I was less nervous about this surgery than my port insertion surgery. I guess because I'd been through the process once before myself (plus watched both my mom and Ben go through their own surgeries recently). That took so much of the fear and unknown out of the equation. Also, I've had over 7 months to get used to the idea of having this surgery, thought I was going to have it in July, and now the time has finally arrived. I've done plenty of reading and research and ultimately, was just ready to do the next step of this process.

Certainly I was a little nervous. What if recovery is awful? What if they find more cancer? What if they can't do reconstruction? But, mostly I was able to put those questions aside and focus on preparing my overnight bag (which I WAY overpacked, of course) and taking care of wrapping up work (I won't be painting for the next two months while I recover) and getting the house and kids and schedule ready for me to be out of commission for a while. That all took most of my concentration and focus for the past week, although I was able to slow down about Thursday and just enjoy just hanging out with the family all weekend, participating in Halloween activities and getting Ayla to all of her club volleyball tryouts that were all weekend long.
We had to be at the hospital at 5:30am, showered with antibacterial soap, no lotions or creams, and all my jewelry removed. Ben was able to come with me and while he did plenty of waiting room waiting, he was able to come into my pre-op area right before I went into surgery and was in my hospital room with me afterward.
Pre-op was very fast, especially since my surgery was moved up from 9:30am to 7:00am. Both of my surgeons came in and talked to me again about what I was having done (bilateral nipple and skin sparing mastectomy with tissue expander reconstruction), and made lots of sharpie markings all over me. The nurses asked a bunch of questions, got me set up with an IV, and the anesthesiologist came in to ask his own questions as well. I think I saw at least 8 or 9 people in this teeny tiny little pre-op area.

Shortly before I went into surgery, they injected a blue dye into my left (cancerous) breast. That dye would show what lymph nodes were closest to the tumor and which ones the breast surgeon would need to remove. We were pretty sure that the cancer had not spread to my lymph nodes, so we were only expecting her to have to take 1-2 sentinal nodes, not an axillary lymph node.
It all happened so fast, I didn't have time to get nervous (and nobody mentioned my nail polish). Before I knew it, I was being wheeled into the operating room. I vaguely remember seeing several people in scrubs bustling around me getting things ready for surgery, but I don't remember being put to sleep at all--just waking up later in a recovery room!
I'm pretty sure I woke up and asked what time it was, which I think I did after my last surgery too. Wonder if everyone asks that? It was about 12:30pm when I finally came to, and I think the surgery was over around 11:30, because that's when Ben heard from the doctors. They kept me in the post-op recovery room for a while longer and I was in and out of awareness. I still felt very woozy, couldn't speak clearly and had a few waves of nauseausness coming out of the anesthesia. I wasn't in pain, but could definitely feel a tightness in my chest.
Eventually they rolled my stretcher up to my hospital room, where Ben was waiting for me. I remember talking to the people transporting me, and asking them how I was supposed to move from the stretcher to the hospital bed (I was able to move over on my own somehow). I think I even made a couple of jokes. At least that's how I remember it. Later, Ben asked me what I remembered from that day and said I was really mean to everyone and especially him! I felt pretty bad about that, because in my memory and in my head, I was very easy going and charming and witty! Oops. I guess maybe I wasn't.
Once I was back in my room, I was still really tired from the anesthesia, and had a couple more waves of nauseausness when I tried to eat or take any pills. In fact, I threw up at least twice, once when trying to take a pill, and once after I had gotten up to go to the bathroom.

I'll spare you the photo Ben took of me leaning over the toilet and throwing up! They switched me to IV morphine for pain killers for a while until I was able to eat a little more and the anesthesia could wear off more completely.

My nurses were all really nice and helpful, and eventually I was able to sleep off the anesthesia a little more and eat some food, though very little. I had some applesauce and tried to eat a peanut butter cracker. My mouth was so dry though that I couldn't hardly get that cracker down! Plus my throat was really sore and voice was hoarse from the breathing tube.

Eventually dinner came and I think I ate a bite or two of alfredo noodles and a piece of broccoli. But mainly, I just wanted to sleep.

When I was awake and coherent enough to talk, Ben filled me in on the doctors report. It sounded like everything had gone very well. The breast surgeon said she was able to get everything out, and the lymph node testing had come back negative, so she only had to take 1 or 2 sentinal nodes. We would have a full pathology report later in the week.
The plastic surgeon said he tried to put implants in directly, but my skin just didn't look ready yet to support them and he wasn't sure about the size, so he decided to stick with the tissue expanders so that I'd be able to give more input in the final size and look.
When he came by the next morning, I was able to see what had been done. I've heard a lot of people are very apprehensive about seeing the scars and their changed body after surgery, but since I did a nipple and skin sparing mastectomy and the doctor was able to fill the over the muscle tissue expanders (just with air for now), they actually looked much more normal than I expected. Not the SAME, but very normal, just taped up and marked up with drain tubes coming out of both sides. They were very very hard though, and numb in several areas, which was definitely weird!

This photo shows a much prettier version of the awful surgical bra and drains I have. I'll have to empty the drains several times a day and keep a record of how much fluid they're collecting and what color the drainage is...for about 2 weeks. Maybe longer, but that seems to be about the length of time most people have them. As long as I'm just laying in bed or sitting down, they aren't a big deal, but when I try to wear real clothes or walk around, it's going to form a very weird lump under everything. I'll have to carry them in an apron or fanny pack or pin them to my clothes and hook them to a lanyard around my neck when I take a shower. Fun, huh?

I was able to sleep pretty well in the hospital and found that I was still just really really tired from the anesthesia. I wasn't too uncomfortable, but would have occasional sharp pains where the incisions were and the surgical bra was pressing on them. I kept up with the pain meds though and mainly felt pretty good, considering.
By Tuesday afternoon, I'd been seen by both surgeons, my vitals had been taken (what seemed like constantly) and the nurse had brought me my discharge papers and instructions and they took my IV out. As soon as that IV was out, I got myself dressed (slowly and carefully) and Ben helped me pack up my bag to go home. I wasn't quite stable enough on my feet to walk out of the hospital, so Ben went down to pull the car around to the front of the hospital and I waited for a wheelchair to take me out.
As Ben was leaving, he found out that OT was supposed to come by to see me before I left, so I ended up sitting and waiting for a while before we could leave. When OT got there, she looked surprised that I was already dressed (I think she was planning to help me to do that). She gave me some quick arm and shoulder exercise instructions, had me show her that I could sit and stand up and walk on my own, and then we were able to head out.
Once we were at home, my main job became to rest, sleep and keep up with my medications. We got a wedge pillow for the bed that will help prop me up to sleep better on my back, and we borrowed a small recliner to put in our bedroom, which has turned out to be absolutely perfect. I'm able to walk around the house easily though, and am just moving slowly and trying not to do anything strenuous.
And one of the first things I did once I realized I could reach my ears with both hands was put all my earrings back in. :) Now I feel like me.

I'll update again in a few days once I go through a week or two of recovery and see how things progress. But so far, so good. Just taking it easy and watching lots of television and taking lots of naps. I feel like a happy old lady in my recliner with my blankets and remotes. I needed a few weeks of rest, and although it's not the most comfortable way to do it, I'm going to try and enjoy what I can!
Double-Mastectomy w/Reconstruction: Surgery Plans
After a false start back in June, we are back on track with a surgery schedule (assuming there are no hiccups between now and then--and let's be honest, this entire year has been an awful case of the hiccups).
I recently met with my breast surgeon (who will do the double-mastectomy) and plastic surgeon (who is in charge of the reconstruction process) and we have a surgical plan and a date -- though I hesitated to give anyone the date in the 2020 world of cancellations and rescheduling.
But here it is: The planned surgery date is Monday, November 2nd, 2020. Its the date I would have chosen if I could have picked it myself, which makes me think it'll probably change. They didn't think it was likely to change, and so we'll plan for that, but clearly I've been jaded by making useless "plans" this year.
As I describe the surgery plan, first you should know that I was given the option of a lumpectomy and radiation, a single mastectomy, or a double-mastectomy. I did not want a lumpectomy because it would leave me lopsided, or require a partial reconstruction with body tissues or implants. I also wanted to avoid radiation if possible, and eliminate the potential for having to have a mastectomy further down the road if recurrence were to happen. My mentality was just do it all now, make them even, and let's try to move on.
Once I decided on a double-mastectomy, I could then choose whether I wanted to do a nipple and skin sparing mastectomy (keeping the nipple and skin envelope for implants) or a simple mastectomy (taking the breast tissue, nipple, and skin envelope and then later reconstructing or tattooing nipples). As explained to me, the medical chances for recurrence were minimal in one option over the other, so it was truly my choice to do whatever I was most comfortable with doing.
Both my oncologist and my breast surgeon said the main goal in deciding is to do what would make me feel most assured moving forward and not look back in 6 months and wish I had done something different. For some people, that means keeping your own natural breasts and monitoring them regularly with mammograms, keeping a watchful eye on any recurrence of the original cancer or other breast cancers. For others, it means removing all the breast tissue, knowing if recurrence were to happen, it wouldn't be local in the breast, which would require a mastectomy at that point (if the cancer were to return in the breast and not elsewhere in the body).
I fell somewhere in-between. Because of the location of my tumor, the fact that it was not in my lymph nodes, and I tested negative for the BRCA1 gene mutation, I have the option of a nipple and skin-sparing mastectomy That means that I can keep my natural "look" with an implant placed inside the current skin pocket. Obviously it isn't quite that simple, but that's the gist.
This procedure does leave a tiny bit of breast tissue behind the nipple, where cancer could technically recur. But, by keeping that little bit of tissue, I will be eligible to continue to get regular mammograms to monitor any changes (which would not be done if all the tissue was removed as in a simple mastectomy). So, I get most of the assurance that the breast cancer can't recur locally and then require a mastectomy in the future, plus the regular monitoring of any new or recurrent local cancer through mammograms, and I get to look "mostly" like my old self when reconstruction is complete. So that's where I've landed. In 6 months, could I regret keeping my nipples? Maybe, and only time will tell. But I felt like I wouldn't regret taking all the breast tissue now, eliminating the need for another surgery down the road if mastectomy then became a must rather than a choice.
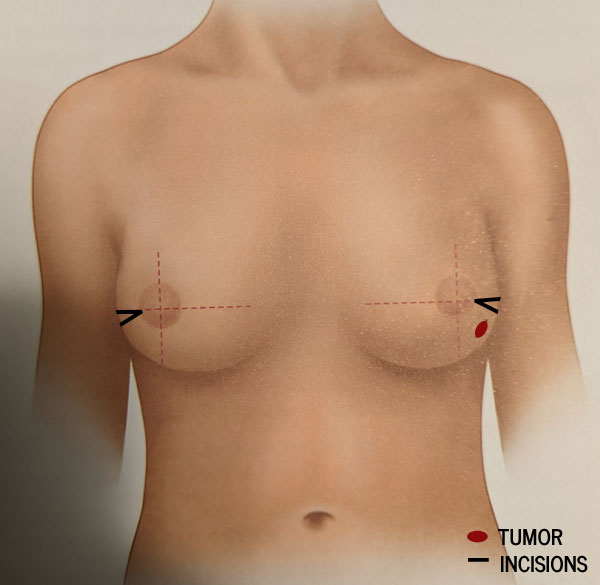
Next, we could start talking about the actual surgery. My breast surgeon describes the mastectomy as a small triangular incision at the sides of my breasts, removing just a tiny bit of skin near where the tumor on the left side was. She'll then scoop out and remove all the breast tissue underneath the skin and behind the nipple, which goes all the way up toward my collarbone. I can't imagine that's a pleasant feeling. Ouch.
She will also remove and test the nearest sentinal nodes (the first few lymph nodes where a tumor drains) and we hope that's all the lymph nodes she has to take. The more nodes they have to take, the higher chance I have to deal with lymphedema, which can be a permanant condition. Since this is on my dominant (left) side, that could potentially be pretty devastating for me. But since my earlier lymph node biopsy was negative, and we're pretty certain the tumor has shrunk down to indetectible on the mammogram, I'm feeling pretty good about what they'll find and have to take.
Then all of the tissue from both sides will be tested by pathology and I will get results back (probably not immediately) telling whether there were any cancer cells still present or anything else concerning in the chest wall or lymph nodes, and whether I will need any further treatment after surgery.
Next the plastic surgeon comes in to do his part -- the first phase of reconstruction. I've chosen to have silicone implants in a two-phase process involving temporary saline expanders inserted over the chest muscle and held in place with a processed "skin subsitute" material that forms a sling and helps hold the implant in place. Then the expanders are gradually filled with saline over a period of weeks or months to stretch your skin to the desired size. Then the expanders will be removed and replaced with permanent implants in a second surgery a few months later. This process is done in two steps to let your body settle and heal from the mastectomy, so you can have a little more say in the size of implants you end up with, and to make sure the tissue is all strong and healthy enough to support the implants and there are no other complications.
He gave me about a 25% chance that if everything looked strong and healthy I could wake up from surgery with the permanent implants already in place and skip the expander process. I'm not counting on that, but boy would that be great to avoid the process that many people have lots of compliants about. I've heard the expanders can be lumpy and hard and uncomfortable and the expanding process can be painful, etc. So, if I can safely avoid that and a second surgery -- I'm in favor. But, it sounded like that's not their usual mode of operation and a more conservative and slower process generally goes better with less complications.
Incidentally, I did not consider a flap surgery to use tissue from my own body (hips, belly, back or thighs) for reconstruction because 1) I don't have that much to give in those areas, 2) it's a much more difficult surgery and 3) I wanted to leave that as an option many years down the road, should I decide to remove whatever implants I get.
So what size will I get? I don't really know, and a lot of it will be determined by the fact that I am doing a nipple-sparing mastectomy. He said "we are at the mercy of where they point." Okay, then--Add that to list of things I never thought I'd hear! I told him, "I'd like to be a little bigger than I currently am, but not so big it's all people notice when I walk in a room," and his nurse laughed. We figure she's seen some excessively large requests! In all seriousness though, because there will be no breast tissue surrounding my implants, if I were to gain or lose weight, my breasts would stay exactly the same size. Since it's unlikely I'll be losing any significant amount of weight (enter possible menopause effects), I want to err on the side of a little bit larger so they stay proportional to the rest of my body.
So, now we wait, and prepare as much as we can for surgery, learn about recovery (which will be between 4 and 8 weeks), and brace ourselves for this next hill in the rollercoaster of a year we've had. I'm very thankful to Ben and his complete support in this process, who does not care ONE BIT what kind of surgery I decided to do--as long as I am comfortable with it.

And ultimately, I am comfortable with this plan. It doesn't remove all worry of recurrence, but nothing would. If the cancer wants to come back, it's going to find a way to come back and there's nothing any of us can do about that. But it won't be for lack of trying to beat it down and cut it out.
Triple negative breast cancer in a localized region after treatment generally has a 91% 5-year survival rate. And actually, my specific MammaPrint results put my 5-year survival percentage at 93% with hormone therapy and chemotherapy treatment. Since my cancer also had a small percentage of estrogen positive receptors, I'll also likely be taking an anti-estrogen hormone treatment pill called Tamoxifen for 5-10 years to prevent any estrogen-fed cancer cells from returning. The good news is that after 5 years, if it hasn't come back, the survival rate increases. Most triple negative cancers will recur within 3-5 years if they recur.
So, we are throwing everything we can at it, and trusting that God is in control and whatever the outcome is, we will handle it, because He'll guide us through it.
Post Chemo Hair Progress
My "pinned" haircuts are looking MUCH different than I would have ever expected these days....

I can hardly believe that hair this short required a cut--but it did! I needed to shape it up a little bit, and try to create the illusion of length on top as I start the awkward process of growing out my hair from completely bald during chemo. First phase -- the fade, which looks a lot like one of my brother Jake's best haircuts.

I'm pretty thankful that my hair is coming back in thick, but I'm still hoping it goes back to it's original dark color and gets curly again as it gets longer. Though I'm not hating the natural silver highlights...

I'm tentatively planning for a progression that looks a little like this, keeping the sides shorter and growing out the top until it's long enough to start going back to my chin-length curly bob.

One thing I did NOT expect in all this hair-losing trauma -- is how much I don't miss the maintenance! No scrunching, no need for 4 different products, no dry time, no brushing or braiding or bad hair days at all when you have a little pixie cut. So, we'll see...maybe I'll stick with short? I don't love the current look, but I like it well enough to work with it--and I absolutely appreciate no longer looking like a cancer patient. I actually get a lot of compliments on my no-nonsense haircut, and it has taken me a while to not feel the need to give a long explanation for why my hair is so short and to just say "Thanks!" I'm doing my best to work with what I've got! It still surprises me when I look in the mirror though.

Though I didn't expect it to (my doctor had warned me otherwise), my hair started growing back about 4 weeks after I finished AC chemo and right before I started Taxol chemo in July. Then, it just never fell out again. I did shave it one last time in July, but it has been coming in pretty reliably ever since.

My doctor looked surprised every couple of weeks when I'd walk into his office with a fuller head of hair than the last time he'd seen me. I'm not an expert, but I kind of wonder how much Taxol was really doing for me, if I was having almost no side effects and my hair was growing in spite of it's presense in my body. Hard to know, but it did seem to play at least a small factor in his decision to let me stop short of the full 12 Taxol treatments because I was having some issues with neuropathy (which by the way have seemed to go away at this point, thankfully.)
Watching my hair grow back feels kind of symbolic in this process. It's a slow outward progression and transformation back to "me", which parallels the slow (and sometimes awkward) internal processing of what the heck I've been through in the past 7 months.
Breast Cancer Awareness

Taxol Chemo #10: DONE with Chemo! 10 Tips for Getting Through It
And I'm DONE --with 12 sessions of chemotherapy!
Since April 2020, I've been through 4 bi-weekly Adriamyacin/Cytoxin and 10 weekly Taxol treatments (we stopped short of the normal prescribed 12 because of some neuropathy that had begun) and hopefully that's the last of any chemo I have to do!
Yesterday marked 6 months since the day I received my diagnosis. In some ways it feels like the longest 6 months of my life, and in others it's like a really long weekend that is finally coming to an end.

I was excited to show up today for my treatment, and decided to dress the part in my breast cancer t-shirt. I brought all of my nurses a couple dozen Krispy Kreme donuts to celebrate (they were supposed to be the fun new fall flavors, but in true 2020 fashion, they were all out) and it feels fantastic to check this off as complete!
Even though this is far from the end of my overall treatment (I have at least two surgeries, reconstruction and 5-10 years of anti-estrogen hormone treatment left to go), it feels like a personal accomplishment to have made it through what was extremely scary and unknown when I first heard the word "chemotherapy". I was terrified of what chemo would do to me, how hard it would be, how sick I would feel, and (keeping it real) what I would look like.
For anyone just starting out on this scary path, I wanted to send out a little bit of encouragement. These photos were taken 6 months apart, during which time I was diagnosed with triple negative breast cancer and completed 12 chemotherapy treatments.
No, it has not always been easy and I did not always feel "cute" or "strong" and there were days that were just plain awful. But after it's all said and done, I'm still ME. The length of time, the side effects, and the changes in my appearance that I was so scared of weren't as terrible as I feared they would be.


- Start off in good shape. Don't wait until you're sick to try and get healthy. Do it now and you'll be in a better position to handle whatever is thrown at you. I fully believe that already having good exercise and decent eating habits (no one is pretending I was a nutritional role model) gave me a huge boost in being able to handle the drugs and side effects.
- Stay well hydrated. People laugh at the gallon jug of water that I try to finish every day (and most days I do!), but I think that was so helpful in curbing my veracious steriod-induced appetite, flushing the chemo toxins through my body, preventing sore muscles and aching joints, keeping my skin healthy, preventing dry mouth, and handling the constipation from steriods.
- Increase protein. Whether it helped or not, I upped my protein intake over the past 6 months and ate lots of baked chicken tenderloin, hard boiled eggs, and a nearly daily post-workout protein powder shake. Overall my nails have remained strong and unaffected, my hair started growing back pretty quickly once I was off the Adriamyacin/Cytoxan regimen, and my muscle tone was able to be mostly sustained.
- Take a daily multi-vitamin. Choose a good one. Take it daily. I believe it can fill in the nutritional gaps where your diet is lacking. A probiotic is a good idea too.
- Eliminate alcohol and reduce sugar. I mean, there's already enough poison in your body. Don't make it harder to recover by feeding it more. I had no problem with the no alcohol portion of this tip, but had trouble in the middle of the taxol treatments with stress-eating way too many sweets. When I cut back, I could tell a significant difference in how much better my body felt and specifically in a feeling of decreased anxiety. That's funny since most people drink alcohol and eat sweets when they are anxious. It turns out those things (over time) make me anxious, and reducing or eliminating them helped me stay much calmer and more even-keeled. Once I realized that drinking alcohol and eating junk food weren't actually solving or relieving my stress (but instead were contributing to it), it made it much easier to resist them--I mean, not always, but more often.
- Get plenty of sleep. A regular bedtime and wake-up time really helps my body run well. I function best on 7-8 hours a night, from 10pm to 6am. When I don't hit that on average, I notice that I start feeling more sluggish, needing more coffee, craving more sweets, and feeling more cranky and irritable. Following each chemo treatment, I allowed myself extra rest and naps to recover (and during AC to just get through the nauseasness and awful-feeling days).
- Get regular exercise. I just enjoy exercise, which I know isn't everyone's favorite thing to do. But for me, being able to exercise 5-6 days a week meant that I felt "ok" and like "me" while I was going through chemo. The physical benefits (energy, strength, posture, reducing muscle and joint stiffness, and flexibility) were almost second to the mental and emotional need I have to being able to move my body everyday. Since I had to take several short breaks from my exercise routine to accommodate the effects of AC chemo and to travel for family emergencies, I could tell that not exercising regularly made me feel much worse than when I was exercising daily.
- Stay ahead of the side effects. Take the stool softeners, anti-nausea pills, claritin and use mouthwash pre-emptively! Your stomach and bowels and joints and mouth will thank you. Hard candy helps with nauseasness. Lotion and chap stick are your friends.
- Delegate to others. You can't do all the things you were doing before chemo began. Killing cancer cells isn't a full time job, but it does require a lot of your time and energy. Some things will have to slide, be postponed, or be done by others. Delegate where you can--and if you're willing to share your experience with others, people will come out of the woodwork begging to help you in any way possible! It's wonderful...Take the help!
- Let go of expectations. Everyone's body responds differently to chemo. What I dealt with may be very different than what you have to handle. But if you go into it with an open mind and no expectations for exactly how it will go, what it will do and how you will respond, you're more likely to be able to roll with and adapt to whatever comes. It's kind of like the first night on a cruise ship....keep your body loose and move with the ship instead of fighting it and you're less likely to get seasick. When your body is tired, rest. When you are hungry, eat. If you are cranky or emotional, give yourself permission to feel that way. The good news is, the cancer card works almost everywhere and people will give you a lot of leeway if you aren't able to do and be all the things you are used to being at the capacity you are accustomed to. Now is the time to give yourself lots of grace and permission to take a break when you need one.
I hope to take that same attitude into my next challenge -- surgery. I will most certainly have to slow down even more, modify my daily life and routine in many ways, and be willing to accept some physical limitations, at least for a season. I feel like going through chemo has prepared me to do that well.
And PS. According to my mammogram in June, the chemo worked and there was no evidence of cancer shown in the imaging. Hopefully that has remained true throughout the past few months and all this is just throwing all medical science has at ensuring we get all the microscopic cells both systemically AND surgically. For now at least, the long term prognosis looks good!
Taxol Chemo #6 through #9
Taxol #6 went well and was uneventful on it's own.

But then life got complicated again.
I skipped a week of treatment between Taxol #6 and #7 because I was in the middle of a(nother) family emergency. I was in Southern Illinois with my mom, who has been dealing with an unexplained infection and was hospitalized in a really unfortunate ending to an epic summer cross-country camper trip. She went from driving her truck and camper across the country with my two kids to being bedridden IN said camper in Southern Illinois with fever and body aches for a month. Everyone (friends, family, and doctors) had assumed it was COVID and told her to quarantine, even though she tested negative 4 separate times! That meant the infection she had continued to grow untreated for several weeks while she weakened.
She was finally hospitalized when she noticed a bump on her chest and still had not improved after a round of oral antibiotics. She had surgery to drain what turned out to be an abcess in her chest and had about a million tests and scans done which have eliminated several things, but unfortunately have yet to provide any real answers for a diagnosis.
After a week in the hospital in Carbondale, Illinois she was moved to St. Louis University Hospital in Missouri for more expertise on her case. After an additional two and a half weeks in that hospital, she has finally been moved to an acute rehab facility in St. Louis. While we still don't have answers for how or why she got this infection or why she continues to have fevers, at rehab she will *hopefully* begin rebuilding her strength and mobility and finish off a 6-week IV antibiotic regimen and continued care for the wound vac on her chest to close up and heal the surgical incisions (we've been told that process can take anywhere from 1-6 months). All of this has been and will continue in St. Louis, where NO ONE in my family lives, including her, which has made it extra challenging and stressful. It's going to be a long recovery process, and I am her main caregiver (though my brother and aunt have been very helpful as well). I am happy and honored to be that for her, but I didn't really have room for that kind of responsibility on my plate this year. 2020 doesn't care.

All of that to explain why I missed a week of treatment because I was in Southern Illinois/St. Louis for a week and a half, then rushed back home to Birmingham to get treatment #7 before heading BACK to St. Louis for another 4 days, only to then rush right back again to Birmingham for treatment #8. It would have been nice to just have my treatment at the SLUH Cancer Center next door to where my mom was hospitalized, but insurance and care doesn't work that way....so I traveled.
I should mention here that my doctor has had no problem with me missing a Taxol treatment week here and there, and in fact that's very common for anyone whose white blood count drops too low between treatments and needs an extra week to recover. So I was not concerned about missing one week, but wasn't personally comfortable missing several or increasing my dosing to go in less frequently for treatments. Since things were going well on Taxol so far, I didn't want to rock the boat, even though my doctor said we could do a higher dose every two weeks instead if I needed to be out of town. I was worried about side effects increasing and wanted to avoid that as much as possible since I'd had basically none so far. Well, maybe not none, but very few and very minor and difficult to distinguish whether chemo drugs or life stress was causing it -- a little fatigue, occasionally having trouble catching my breath after workouts or walking up big flights of stairs, some very vivid dreams, increased appetite and slight weight gain (from a combination of steroids and stress eating, for sure).
After treatment #7, I was only home for a couple of days, so I spent the day after treatment working and painting signs before I left town again for an indetermined amount of time. I noticed while I was painting, that I was having trouble using my fingers and thumbs to pick up letters and to hold my paintbrush. It was subtle, and I was preoccupied, but I did notice what was probably the first signs of a Taxol side effect -- neuropathy -- the side effect I've been most concerned about from the beginning on this type of chemo. I didn't think much of it that week, since I had so much else on my mind, and headed back to St. Louis for more hospital time with my mom.
I did notice that throughout the following week my hands and elbow were hurting much more again, cramping up and having joint pain. My feet were also beginning to hurt more, the plantar fasciitis in my arches was acting up again, and the balls and heels of my feet felt bruised and sore. I began having trouble during my workouts with some of the faster running and side-to-side transitions that didn't used to be an issue and even more trouble gripping and holding onto dumbell weights than normal. I assumed that was from the several extra hours per day on my phone and texting, and from jumping and doing HIIT workouts on concrete and hard floors (instead of that lusciously bouncy Burn floor). And ultimately it's entirely possible that's all it was causing those ailments -- I just can't know for sure.

I've gotten tired of masked photos, so the strategy is this -- get a long drink of water from my giant water jug and THEN take my weekly photo before I put my mask back on for the rest of the treatment session.
But, after Taxol #8, I was definitely having noticeable numbness, tingling and pain in my hands, fingers, toes and feet, particularly on the Saturday and Sunday immediately following that treatment. I may have freaked out a little bit--or a lot. Neuropathy can get worse with each treatment and while it *can* improve, my hands are my livelihood and the thought of 4 more treatments hindering my hands and feet even more made me very nervous....especially since IF it was reversible, that could take months. I had an appointment with my oncologist the following week (right before Taxol #9) so I planned to visit with him about what the best plan moving forward would be.
Also, after #8, apparently I missed my window to fall asleep before the steroids they gave me kicked in at full speed, because on Friday night I was awake until after 5am! That was the first real insomnia bout that I've dealt with so far, but that can be really common. I did end up sleeping about 4 hours that Saturday morning, but then stayed awake the rest of the day and continued to feel the amped up highly caffeinated steroid effects through Monday. Unfortunately I wasn't able to channel that energy into anything productive because I was having trouble focusing and trying to rest and de-stress (not work), so I finished up watching the rest of season 4 of This is Us instead.

Then there's the hair situation. Though I've heard that you are supposed to continue to lose your hair on Taxol, that has not been the case for me. While it's not exactly growing fast, my hair is definitely growing. It's not the right color or texture yet, and maybe it'll need another buzz before that comes in, but it's definitely still thick and not patchy, so I'm very grateful for that!
Now I feel like instead of looking like a cancer patient, I look more like I chose this no-nonsense haircut. Frankly, that's exactly the kind of haircut I've needed this summer with all that's been going on in our lives. Even though it doesn't quite fit my personality or look like I'd like it to look (I mean, I had some good hair pre-chemo), I've appreciated the fact that it's been slowly coming back. To think I expected my hair loss would be the most difficult thing to deal with this year! Since I shaved it all off back in May, I've barely given it two thoughts since I didn't expect it to be there at all, and by the time life calms down for me to really notice it, it might be time to try and put some kind of style into it!

Which brings us to Taxol treatment #9, which I'm currently receiving as I write this. I had an appointment with my oncologist today and when he saw my head full of hair and heard my concerns about increasing neuropathy in my hands and feet, he decided two more treatments would be enough. He seemed a little surprised that my hair had grown so much, and mentioned that because I was on a low dose of Taxol and it wasn't causing any hair loss, it wasn't going to be productive to reduce my dosage and continue through the rest of the 12 treatments. Instead, he said he wanted to do today's (#9) and next week's treatment (#10) and call it complete.
I can't say I'm too disappointed in that cancelation in 2020.
So, now I will hope that the neuropathy doesn't increase much (or at all) in the next two weeks, and then we'll go back to discussions and planning with my surgeon for the next phase of treatment--surgery. I've learned not to put firm dates or expectations on anything this year, but if you're looking for a ballpark timeline, I'd say it's *possible* I'm looking at having a double-mastectomy surgery and the first phase of reconstruction as early as the end of October 2020 -- just in time for Breast Cancer Awareness month.
Overall, I'm feeling pretty good about how all of this has gone and is going. With all that has been happening in the world and in our own family, I just haven't had time to worry about whether the cancer is still there, if it will grow, if it will come back, if treatment is working, etc. I've just been following the treatment program and letting the doctors and drugs do their thing without worrying about it. Maybe that's ultimately a blessing. I've had no time to fret about that because there have been way too many other things to emotionally respond to this year--
- a pandemic
- my father passing away
- job insecurites for both Ben and myself
- my mom in the hospital in a state none of us live in with a mystery infection that can't be diagnosed
- COVID policies and procedures dictating our lives everywhere we turn
- a staggered in-school and virtual hybrid schedule to navigate.
As many people have said to me with a look of shock and pity and empathy over the past several weeks -- That's a LOT. And it is. But thankfully I'm not carrying it all myself. Somehow, some way, God will get us all through all of this and he'll take care of us exactly how we need to be cared for. We've seen it already in about 1000 ways, so I'm trusting that will continue, and I'm not worrying about making sure it looks the way I think it should. It's just not my show to produce.
I joked to several friends recently that if I'm supposed to learn that I'm not the one in control this year, consider the lesson learned!
John J. Nokes: Cancer in Common
Just a couple of weeks ago, on July 19, 2020, my father passed away from cancer. That's not easy ANY time, but it sure is a punch in the gut when you're also going through your *own* cancer treatment.
Daddy was originally diagnosed with cancer in the summer of 2019, and went through chemo and radiation last fall. His cancer responded well to the treatment and his prognosis was good, with a 95% success rate. While his treatment was aggressive and very difficult on his body, throughout the winter, he was feeling better and improving in energy and endurance every week. In December 2019, he had clear scans and we were making plans to see him in April 2020 in Tennesee for a volleyball tournament.
When I was diagnosed with breast cancer in March 2020, he was the person I wanted to talk to about it. While his cancer was different, he had recently been through similar treatments and had to face the challenges of getting physically sicker and weaker in order to get better---something I was terrified for in my own life.
Daddy and I are a lot alike. We don't like to depend on other people. We want to be strong and capable and nonburdensome. He was encouraging to me. He told me to take it one day at a time--have just one goal for each day. I took comfort in knowing that if he could do it, I could too. (I also vowed to allow people to help me and to let people into my experience -- something I didn't see him do much of, but that I knew was important for me to do in order to get through this well.)
When he told me in late April that his cancer had returned and spread to other parts of his body, it was a devastating blow. Not just because HE was facing metastatic cancer and unsure about what his future looked like, but because his predicted success rate statistic after his treatment was high (95%), and so is mine (93%). Statistics don't matter for anything other than knowing what the most likely best route is to take for treatment. What happens to YOU and your cancer doesn't care one bit about the statistics. It's impossible for me not to compare...and that was hard. Is hard. And will continue to be a weighty pressure on me.
Is it strange to say though, that because I'd just been faced with my own mortality through my diagnosis, while he was also facing his, I was able to bond with my dad in a way I don't think anyone else in the family was able to do in those last two months. As he began his radiation and immunotherapy treatment, and had his head shaved because of hair hair loss, and while I was going through the worst weeks of my AC chemo treatment, we spent May and June talking pretty candidly with each other about how we felt, what we were each going through, and accepting and making peace with whatever each of our lives would look like moving forward.
I understood him when he said he'd had a good life and he didn't want to prolong miserable treatments and suffering in the name of living if it wasn't allowing him to *really* live. He didn't give up. He didn't give in. He was just ready to go when it was time. Even though I am his daughter and I wanted him to live a long healthy life, I was able to step into his shoes and know exactly what he was feeling and understand it--from *his* perspective, not mine.
So, when the radiation treatment just couldn't keep up with his cancer and complications began that put him in the hospital only one treatment into the immunotherapy that we *hoped* would prolong his life, my prayer for him was simple -- "Please heal him so he can LIVE and be the Chief he wants to be, or take him quickly so he won't suffer long."
My prayer was answered--not with my first choice of response. But because I *knew* Daddy was ready, and didn't want him to suffer, I was at peace with the answer we were given...and I know he was too. "Keep the faith," and "I'm in God's hands," are phrases he'd repeat often.
I never could have had that feeling of peace without also going through my own treatment at the same time. We never would have had those last real, candid, and honest conversations without our circumstances being what they were.
So, in the middle of my own grief and this jacked up, messed up, tragic and chaotic world of 2020 (that I pretty much HATE), I'm also immeasurably thankful that Daddy and I had cancer in common.