Andrea's blog
Elbow Surgery - Golfer's Elbow & Lacertus Syndrome

I thought it had been too long since I had a surgery...
Not really.
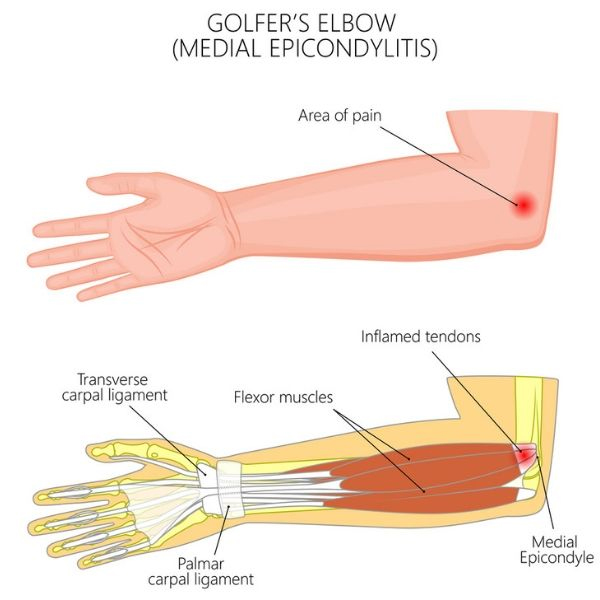
But after all my breast cancer treatment and surgeries were complete this spring, I realized that my Golfer's Elbow injury from tearing apart an enormous fence two years ago *still* wasn't any better.
The initial injury...

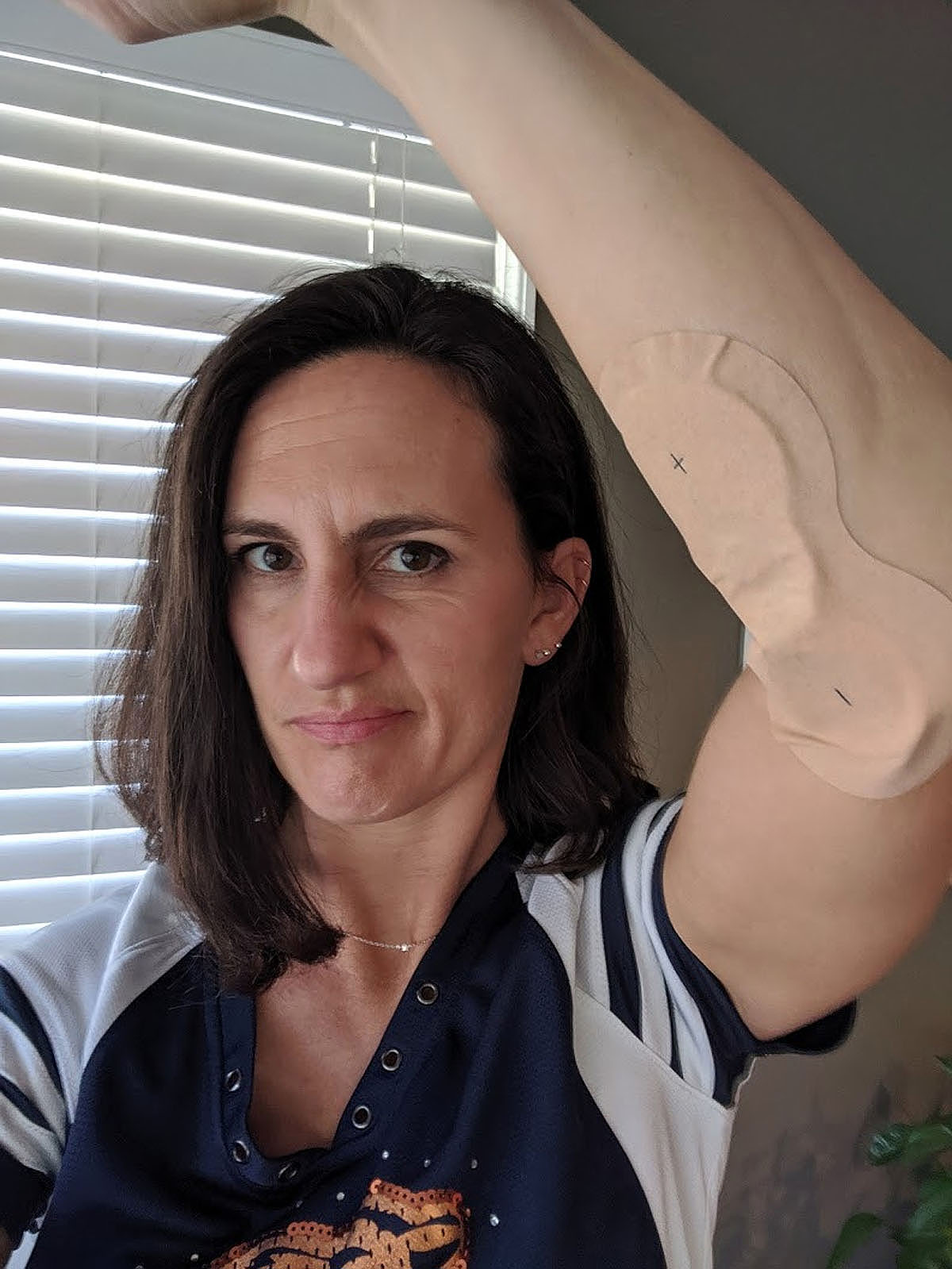
I've tried physical therapy exercises, dry needling, rest, a cortisone shot, plasma rich platelet injection, a wrist brace, elbow compression sleeves and lots of modifying for daily activities. But it just wasn't going away.

Dry needling efforts...

Compression sleeves and lots of modifications...

Platelet-rich plasma therapy injection...

Wrist brace...

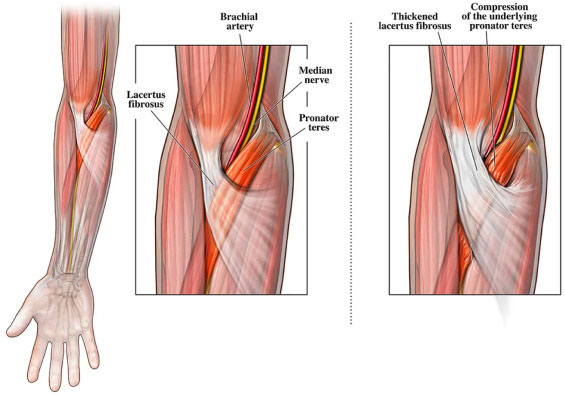
I finally talked to a surgeon a couple of weeks ago, who diagnosed me with both Golfer's Elbow and Lacertus Syndrome.
It turns out the Lacertus Syndrome (a fairly rare condition, often seen in throwing athletes) is an unnecessary band that was restricting the muscle in my forearm and keeping it from expanding when it was exercised. It finally made sense as to why the PT exercises to strengthen my forearm muscles to solve the Golfer's Elbow weren't working.

Done.
Exactly one year ago (on St. Patrick's Day 2020) I received a phone call that stopped me in my tracks and flipped our entire world upside down. Cancer.
It has been a long, all-consuming and difficult process, including 5 months of chemotherapy, three surgeries, the trauma of complete hair loss, large chunks of time where I felt physically sick and weak, mentally discouraged, and frustrated at having to put so many things aside to focus on the task at hand. Whether I wanted it to or not, everything we did for the past year had a wrapper of cancer treatment around it. I was either anticipating, going through or recovering from some step in the process, waiting for the next appointment and the next unknown.
But as of this week--it's over! I'm finished.
As I had my stitches removed from my final reconstructive surgery on Monday, I sensed a dark cloud that has followed me for a full year roll away. The skies above me cleared and I felt like I could finally look up and forward and see life beyond this season. I cannot adequately describe the incredible feeling of relief that washed over me, and frankly took me completely by surprise.
Ben, my lifelong DJ, suggested I take another listen to the song "Rainbow" by Kacey Musgraves. I could not keep the tears from rolling down my face as I listened to the words...
As a family (both immediate and extended to all of you who have walked alongside me), we are not left unaffected by this storm-- but we are through it. Finally.
So today, instead of forever associating St. Patrick's Day with a grim and heartbreaking day that hijacked a full year of my life, I'm able to smile and laugh and look forward to a lighter and brighter future.
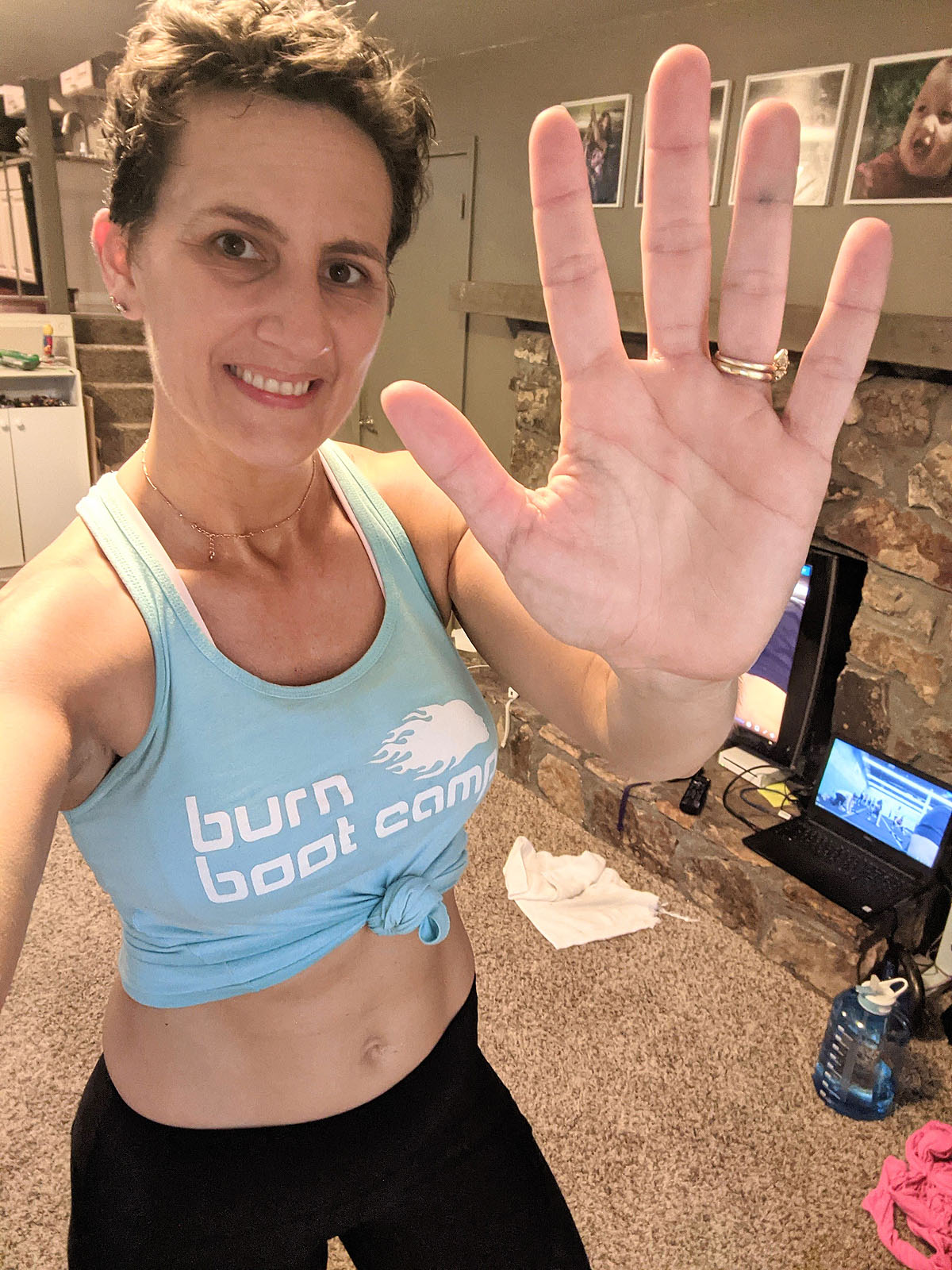
And this shirt seemed perfectly appropriate to sum up my year...

Exchange Surgery, Fat Grafting, & Week 1 Recovery
The short version:
- Surgery went well.
- Fat-grafting is much more significant recovery-wise than the implant exchange has been so far. I am still very swollen and sore at the fat grafting donor site and where it was injected, but my new breasts and incisions aren't bothering me much at all other than being a little itchy from the surgical tape.
- My arm mobility is almost 100%, although I'm intentionally not over-extending or lifting more than 5lbs to allow my incisions to heal.
- At one week post-exchange surgery I feel more like I did 4 or 5 weeks after my previous surgery, so it's significantly more tolerable this time around.
The longer version:
Surgery Day
Ben and I got to the hospital around 6am on Monday, surgery day. I really wasn't too nervous about the process this time. Just ready to get it done and put it behind me. Surgery day itself is pretty easy for me. I just have to show up. Everyone else is doing all the work!

I brought significantly less stuff with me this time, since I would be going straight home afterward that afternoon--basically just the clothes I was wearing, my phone and my Kindle. I was glad that I brought my book to read while I was waiting back in the pre-op area though, because they didn't let Ben come back there until after I had gotten my IV and talked to the doctor, which was almost two hours after I went back. So, I guess I was pretty chill since I was casually reading fiction while I waited...
When I talked to my surgeon, he re-explained what we were doing -- exchanging my tissue expanders for silicone implants, pulling both my breasts in just a little bit to have less of a gap between them, removing my port, and fat grafting from my lower back and inserting it into the upper cleavage to soften the edges of the implants, since there was no breast tissue to do that naturally. I told him I liked the size we'd gotten to with the expanders, but I didn't care so much about what size they ultimately were, as long as they were fairly symetrical and "fit" my body. I think it's helpful in this process not to have too specific of a picture in your mind of what they will look like finished. For me, that leaves less room for disappointment, and more likely to be accepting of the final result.
One thing to note (should you be going through this), is the amount of saline in the expanders does not necessarily translate the same number of CCs for the implants. So, although I had 300cc of saline in each breast in my expanders, I knew in order to achieve the same size with silicone implants, they would likely be a larger number. I didn't have the opportunity to choose which kind or size of implants I wanted. I trusted my surgeon to pick the right size based on the way the expanders looked and our conversations. So, of course my first question when I woke up in the post-op recovery room was "What size implants did he put in?" And I had to ask twice, because I was completely drugged and incoherant and didn't remember the answer the first time.
But, I got my answer: 415cc on the left and 385cc on the right. The implants I ended up with are Natrelle Inspira SoftTouch SSF by Allergan, which are one step below the highest profile (roundest) option, and described as "smooth, full profile". It's not uncommon to have two different sized implants in order to make them symetrical. Since natural breasts are rarely exactly the same size (mine were not), one side might need a little larger implant to match the other. The size and type of implant is really determined more by your chest width and size of your chest cavity. I've read stories from other mastectomy patients that said they had 700cc implants and ended up a small C-cup. Clearly 700ccs would make me look enormous, but on someone with a wider chest and deeper chest cavity, it might not be very large at all. It's also worth noting that the number of CCs of implant used for a reconstruction has a completely different meaning than a breast augmentation, which would be adding the size of the implants plus your natural breast size. The point is, don't get caught up in the numbers. They mean different things on every person's body.
But really, beyond collecting that information (and the time...I always want to know how much of the day has disappeared when I wake up from surgery), my main focus was to try and wake up and evaluate my pain levels.

It took me a little while to not feel so groggy, and they let Ben come back with me before too long (the details are fuzzy now). I do remember having a very dry and sore throat from the breathing tube, and feeling VERY nauseaus. I threw up several times before we left the hospital. Evidently that's my typical response to the anesthesia. I wasn't in too much pain, though I could feel that my chest was very sore, particularly the top portion (where they added fat). My lower back was mostly numb, so it wasn't bothering me much (yet).

Once I was feeling pretty alert and had finished throwing up, they let me get dressed and leave--in a wheelchair of course, which I was thankful for, because the walk from my hospital bed to the bathroom was pretty shaky.
We got home a little before 2pm, and I went directly to bed, propped up on my pillows. I was able to check my phone and text a few people, but my throat was hurting so bad, and it was hard to swallow and I kept falling asleep. In fact, I fell asleep sucking on a cough drop. Thankfully, I didn't choke on it, but it was still there when I woke up an hour later. I was able to eat some yogurt and scrambled eggs that afternoon, but anything more solid than that was impossible for me to swallow.

When I woke up later in the afternoon, I had a rude awakening. The numbness on my back was wearing off and OUCH. Suddenly the soreness there was MUCH worse than my chest. I took pain pills pretty regularly through the next evening, which definitely helped, but when you can't lay on your side or front, and your back is sore, there's nothing super comfortable. I ended up piling pillows on top of the wedge pillow, leaving a gap at the bottom so my lower back didn't rest directly on the pillow. That kind of worked. But then all my bodyweight was put on my bottom and my tailbone, so eventually that gets sore too. Getting up and walking around a little bit every once in a while was a good relief.
That evening, I was able to change clothes and take a look at myself and see what kind of damage had been done. I noticed immediately that my arm mobility was significantly better than it was after my mastectomy surgery. I had no problem changing my clothes myself, though I did it slowly and gingerly, and though I wasn't going to fully extend, I could lift my arms enough above my shoulders to reach the overhead light switch in our closet, items on the closet shelves, etc. I saw that my waist was very bruised, a little swollen, and I had two small stitches on my back from where they did the fat grafting.

I'm supposed to wear a bra 24/7 for the next two weeks at least -- maybe longer (hopefully a more normal-looking one than this surgical vest that looks terrible and lumpy under every item of clothing). My chest is taped up with clear tape, so while I can kind of see what I'm working with (which looks fine--different, but fine), I haven't focused much on what my new breasts will look like until the tape is off and everything settles down and into place.
I did notice though that my surgeon did not use my mastectomy incisions for the exchange (which were on the sides of my breasts, kind of like sewing darts on a dress). Instead, he made new incisions below each breast, which explained why I had some dull pain there. I had assumed he'd use the same incisions, but I guess he decided this was better. Once they heal, I don't think they'll be very noticable, but I was a little bummed about now having two mastectomy scars, two exchange surgery scars, two drain scars, a port surgery scar, and two new small scars on my back. That's quite few battle wounds from this year.
Week 1 Recovery
I spent the next several days on the couch during the day and in bed at night, propped up on pillows, and just taking it easy.

I was still taking pain meds and antibiotics, and so my main job was remembering when to take my meds and trying to avoid the post-surgery and pain pill and lack of movement-induced constipation that is inevitable. TMI, I know, but it was a huge part of the first week of recovery and is VERY uncomfortable. I took stool softeners and HerbLax supplements, drank coffee and lots of water, and eventually that worked and I had some relief. It's also an incentive to STOP taking the pain pills since they cause a lot of that, so by Wednesday morning, I was only taking tylenol for pain. The pain pills also make me itchy all over, so that was another incentive to quit taking them.
I did lots of reading on the couch, and just trying to be patient and let my body put ALL my energy into healing. I was surprised at how good I felt compared to the last surgery. Not having drains is a gamechanging difference and were it not for the soreness and swollen feeling from the fat grafting, I think I would have felt amazing right away. I was able to do pretty basic tasks like making coffee, emptying the dishwasher, and heating up my own food, etc. which were good ways to get me moving around a little bit each day. Walking around definitely hurt at first, because of the bruising, but each day lessened a little bit, making it easier to move around.

While the bruising on my back and sides went down and didn't look too bad, my lower back became much more swollen and has stayed that way the rest of the week and has by far been the main focus of this recovery. It feels like I have a fanny pack attached to my back. It's numb in some spots, tender to the touch, itchy as nerves come back to life, and my waist feels about 2 or 3 inches wider than it normally is. I barely notice my incisions from the exchange, but I definitely feel the bruising and tenderness where they inserted the fat on my upper breasts. I hope the fat grafting "takes" because I'm not interesting in signing up for this part of the process again, which is an option down the road if I'm not happy with the results. I'm gonna have to be REAL unhappy with the results to do this again though.

Thursday and Friday I did some work at my desk in the mornings, and then spent the rest of the afternoon and evening on the couch resting and reading. Physically, I am definitely tired and moving slower than I normally would, but mostly I'm feeling good. Mentally, I am doing MUCH better than I was after the last surgery. I know it'll just take time and I have to be patient, but everything will feel "normal" again eventually.
By Saturday, I was ready for my first trip out of the house, and went to Ayla's volleyball tournament, here in town. It was admittedly ambitious, especially since it required quite a bit of walking from the parking lot to the court & back. But I decided to take a pain pill to get me through it, which was a good choice.

Sunday, I was able to drive myself to the tournament (no pain pills that day) and sat through several matches as well as lunch at a restaurant with Ben's parents. By the time I got home that afternoon, I was pretty exhausted.
This week, I expect to be back to a mostly normal workload and daily responsibilities. I can accomplish most of the things I need to do without too much physical activity, so it'll still be a pretty restful week. I don't expect to be cleared to exercise for at least 3 more weeks while everything heals and settles into place, so I'll continue to lay low until then.
I'll see my plastic surgeon's nurse next Monday and be able to take the tape off my incisions at that point. And hopefully the swelling will be down by then? We'll see...
Preparing for my Exchange Surgery
Mid-February put me 3 months post-surgery after my double-mastectomies and first portion of breast re-construction. I had a meeting with my plastic surgeon to check on how everything had settled and begin talking about the next (and hopefully final) phase -- exchange surgery, which has been scheduled for this Monday, March 1st.*
*It's worth noting there, that my initial ultrasound and mammogram was March 2nd, 2020, so this final step will happen *just* under a full year from the time we first started this process. This ain't no boob job...

The next surgery is called an "exchange" surgery because they will be exchanging the strange-feeling and looking, hard as rocks tissue expanders with silicone implants that they assure me will look and feel much more natural.
In addition to the implant exchange, my surgeon will be removing my port (YAY--while I was glad to have it, I won't miss looking at that bizzare contraption!) and doing something called fat graphting. He calls the fat graphting "photoshopping", but as a regular user of Photoshop, I KNOW that digitally photoshopping is NOT the same as having fat sucked out of one portion of your body and inserted into another. Photoshopping doesn't hurt. But, I get his point, and it does help explain WHY he's doing it. Since I won't have breast tissue above my implants, they can take fat from another area of my body (my lower back "love handles", in my case) and insert it into the layers of skin above the implants to soften the edges of the implants under my skin and make my constructed breasts look more natural and less like they're just two half softballs stuck to my chest.
I'm skeptical about the benefits of fat graphting vs. the pain in recovery and bruising and compression gear required for several weeks afterward, especially since I've been told it may take several separate attempts at the fat grafting for it to "stick". A large percentage of the fat moved often doesn't "take" and re-absorbes into your body. But, for this surgery, since I'll already be put under and have forced recovery time, I figured it was worth an effort if he thinks that will help it have a better finished result. I gotta trust him. He's the pro.
I was very glad he didn't ask me to gain a bunch of weight before the surgery. I was just hitting my stride with 5 good HIIT workouts a week. I did eat plenty of Edgars orange rolls though over the past couple of weeks, because why not?
Over the past 3 months, I have VERY much enjoyed getting back to full functionality, and I'm not looking forward to another 4-6 weeks of sitting still and recovering. But I am VERY thankful to be knocking out the next, and hopefully last, big step in this cancer treatment journey.
I've spent the last week getting ready to be out of commission again for a while, and while I definitely have some anxiety about going through another surgery and recovery, this is a WHOLE different ballgame. At the end of this surgery's recovery, I should look better, not worse (which was definitely the feeling after my port insertion and double-mastecomy surgeries.) There's not a fear of what the pathology will say, and it doesn't even feel that "cancer-related." It's also the last step in a LONG list of steps that I've been going through one at a time over the past year, which feels pretty good.

The way I see it, I've made it through all of that, so I can surely get through this too. Here we go...
Back to Work
My work life has been severely interrupted in the past year, by cancer treatment, COVID, virtual school, my father passing away, my mom being hospitalized for two months in another state, and then my own surgery and recovery.

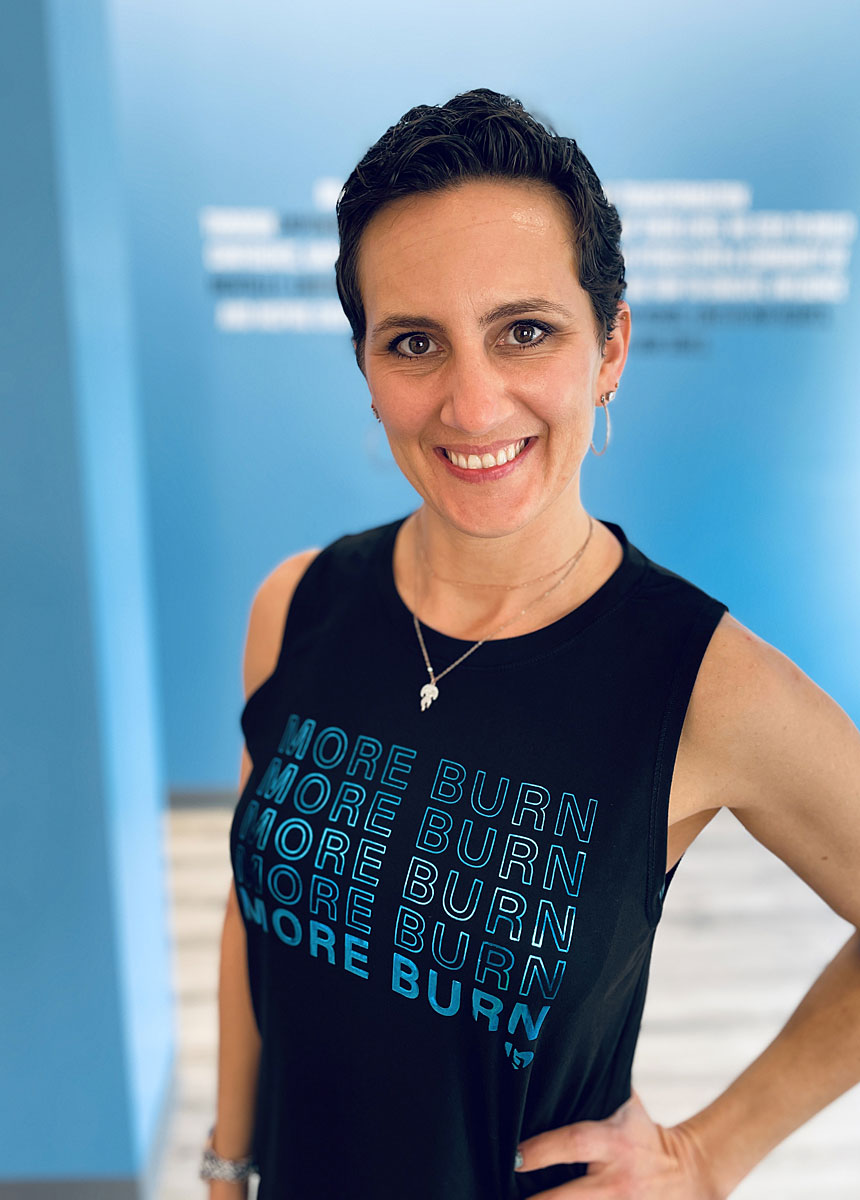
Over the past month, I have thoroughly enjoyed getting to (again) work with some of my closest friends and having the opportunity to combine my interests and talents to promote health and confidence to women in our city. We have a VERY talented team (not all pictured below) and it's an honor to be able to work alongside them. This past month we launched the new gym in Homewood, and even in the midst of the struggles that come with running a business in the pandemic, it has been a raging success in it's first month, largely due to the talent and diligence of this team.

For me, it's been a wonderful (and welcome) return to socialization and working on a team, and thinking about OTHER women and their health instead of just my own!
And, while it has taken me a little longer than I expected it to, this past week I have finally felt ready to return to painting signs. I painted my first round of the year this week, and it felt very good to create something with my hands again!

Whether or not the feeling lasts (because I've learned not to count on anything until it happens), it finally feels like I'm gaining my footing back and feeling like ME. I'm looking forward to fun things in 2021...as long as it continues to cooperate!
9 Weeks Post-Surgery
Today is about 9 and a half weeks post-surgery. Thought I should give a little update, and show off my curly pixie haircut (which is about 6 months of growth from completely bald in July 2020)!

Cancer Treatment. I saw my oncologist, who was very pleased with my surgery pathology -- no evidence of cancer! Clearly the chemo was successful. Because my initial tumor was slightly estrogen positive, as one last attack and prevention method, he recommended I take Tamoxifen, an oral estrogen receptor modulator, probably for 5 years, as long as the side effects of it don't radically affect my day-to-day. I had thought it would be 100% required for me to take it, and I expected to be taking it for 10 years. I was also very nervous about the horrible side effects I've heard and read about. But, his "try it, and if you don't have severe side effects, take it for 5 years just to be sure we did ALL that we could" prescription sounded good to me! I'm going on almost two weeks on it, and so far haven't noticed a thing as far as side effects. He said it could take a month or two to see how it affects me though. So, stay tuned on that front...
Reconstruction. As far as my breast reconstruction process, the saline fills in my tissue expanders were pretty easy. I ended up with three fills, and am currently as large as I care to be at 300cc per breast. These tissue expanders are still really strange feeling and hard as rocks, with little air pockets in a couple of places. I'm extremely thankful these aren't the final product, but at this point they are tolerable, and not painful, and to be honest, I'm enjoying the rest of my body feeling GOOD enough that I can happily hold off a few months before facing a second surgery. The implant exchange surgery will be a nice finale to this treatment plan though. I'm currently very happy with my decision to reconstruct and though my breasts won't be the "same" again, they'll be just fine once it's all said and done.
Physically. My last post was written at 5 weeks post-surgery, and I had just started to do some really low-impact exercises and stretching and walking. My body has steadily improved week over week and now has returned to what I consider to be normal--not quite as strong or as fast as I was back in March, but plenty sufficient for a 41-year-old who has had the year I've had! I do have some sore tendons or something under my left armpit that seem to be surgery-related, but it's minor. And my left hip cracks and pops every time I do a squat. I wish I could inject some padding or lubricant into my hip-joints to make that stop. It doesn't hurt. But it's loud.
(7-weeks post-surgery, not at real-time speed of course, but feeling pretty strong!)
I spent week 6, 7, and 8 slowly increasing my workout length and intensity and working on flexibility, and this week was able to do all five of the Burn workouts for the week with just a few modifications--mainly to accomodate my bum elbow* that still hurts from an injury a year and a half ago. My endurance and strength otherwise feels pretty good.

*Clearly the plasma-rich platelet injection from last winter did not magically fix my elbow. Perhaps that's because right as it started to feel like it was really healing, I was diagnosed with cancer and COVID shut our world down, and I pretty much quit all physical therapy exercises for it. I had other things on my mind...
Mentally. While I still don't feel like my brain works as quickly as it used to, I haven't felt nearly as foggy or uncertain as I initially did as I was healing from surgery and chemo, and all the stress from 2020. I just seem to need more time to think, more time to process, more time to plan, and more time to do every task. But in a way, that's been kind of nice--to allow myself to do less, and expect less of myself each day. My pace has slowed down, I feel more focused, and am more willing to stop and sit and look around a little bit instead of just moving full speed ahead. I did a lot of puzzles over the Christmas break.

Emotionally. As my physical body has improved, my emotions have followed. I've been happy. Content. Downright pleasant. I still have bouts of anxiousness, especially in any kind of decision-making for the future situation (which feels wobbly at best). But, even though many circumstances haven't changed, or have gotten harder or more complicated, everything doesn't feel so sad and hopeless and tragic. I'm able to see the bright side a little more often, have a positive attitude again, and tackle problems a little bit at a time instead of being completely overwhelmed by them.
Socially. COVID is still a real drag on my social life, but we were able to pre-quarantine and see Ben's family over the Christmas holidays, which was blissfully almost-normal. I've started working with a couple of my closest friends on a project, so I've been able to see them some (who have all already had COVID) and interact with them on a more regular basis, so that has definitely helped. COVID seems to be *everywhere* right now in our area, so our family is staying to ourselves most of the time, and wearing masks more regularly. It would be really great NOT to get it...so I'm doing my best to avoid it.
But otherwise, we are trucking along pretty well, cautiously looking around the corner to see what 2021 has in store...
Easing Back into Life
Here I am, 5 weeks post-surgery, 1 week after my last drain was removed, and what do you know? The doctors weren't lying. Four weeks was the turning point...

The first few days were rocky though. As I started to cautiously ease back into more normal activities (like driving and laundry and dishes and cleaning and cooking and other REALLY basic everyday activities), I found myself second-guessing every request, every commitment, and every task. "I want to do it, but am I capable? I think I can now, but will I be able when the time comes? Will I have enough time? Enough energy? Enough mental capacity to handle it?"
Normally, I'm extemely confident and sure of what my capabilities are. If I say I can or will do something, I will--end of story. But suddenly, I found that while I'm not completely incapable of everything, I definitely am not able to keep up with my old pace of life. So I don't intuitively know how much to commit to or how much time to reserve for every task, and it's hard to account for my mood changes...of which there are many.
It's a very odd feeling not to trust myself. I don't trust that the "right now" Andrea will feel the same as the Andrea three days from now (or even three hours from now). Everything takes a little longer than it used to (sometimes a lot longer) and depletes a little more mental and physical energy than I expect it to. So that has taken some adjusting, and some trial and error, to see just what the current version of me is able to do everyday. Needless to say, I've had to go very slow so I don't get myself in a pickle and become completely overwhelmed.
I've found though, as the week progressed, my physical and mental state and confidence has improved every day as I've found "success" in various activities.
Physically, I'm definitely improving. I'm stiff and still a little sore and uncomfortable, but I'm not hurting anymore. I've spent a good portion of each day focusing on stretching and physical therapy exercises to increase my flexibility and mobility. I've needed that particularly in my shoulders and arms after surgery, but my legs have done nothing for a month too, so they're pretty tight these days as well. I've been able to do some some low impact bodyweight exercises and walking to slowly ease back into working out. I'm focusing on taking small, slow steps forward so that I don't hurt myself. I've been able to see progress pretty quickly, particularly in flexibility, which has been very encouraging.

I'm not there yet, but maybe in a couple of weeks I'll be back to doing my 4-5 day a week Burn workouts (modified though, for sure). For now, I'm thankful for modified 15 to 20 minute BenderFitness.com workouts, SaraBethYoga YouTube stretching videos and the walking path around the park behind our house.
Mentally, I've started trying to exercise the creative and business side of my brain again, while doing some work at my computer. While it feels a little like I'm stumbling around to remember what I'm doing, it's been a good way to slowly transition back to work-mode before I have to hit the ground running. I'm saving any physical sign-painting work until after the new year, just to give my body plenty of time to heal and to see what kind of energy levels I have each day.
Multi-tasking and thinking about more than one thing at a time is much more difficult for me right now than it used to be. Maybe that's long-term effects from chemo? Maybe it's just from the stress of the year. Hard to say. The more I do though, the more confident I feel about being able to manage my workload. Most days. Some days I fall apart and am overwhelmed...
...which takes me to...
Emotionally, I'm slowly doing better each day, and I'm starting to stack up some good days finally. But still, I never know when or why I might just burst into tears or have a sudden pang of anxiety or dread. I had a complete fall apart about a Christmas tree I ordered from Amazon (after hours of research) arriving WITHOUT A WAY TO PLUG IT IN and said "Christmas is cancelled. We aren't decorating." And I would have stuck to that too...but Ben saved Christmas and found a better looking, less expensive, more fabulous tree at Home Depot and brought it home by the time I had dragged my defeated and angry and depressed self out of bed and downstairs the next day. True story. And yes, Amazon accepted the return. And we did end up decorating for Christmas (cheerfully). The point of that story is that any little thing has the potential to set me spiraling. I can't always control it, though I do try to throttle it from destroying everyone in my path.
...which is a good segue to...
Socially, I'm REALLY struggling with how to be social (which I need) and see my friends and family again in the middle of the COVID-19 pandemic situation we have found ourselves in. While I'm trying to go back to "normal" -- normal isn't there to go back to! I can't just get together with a group of friends or our family for dinner or to hang out at their house, or meet up for coffee or a project without thinking about ALL THE COVID crap.
While I'm pretty sure my family are all very low risk for serious side effects from getting Covid, I have inconvenienced them enough this year and would feel terrible to be the one to bring it home and force our whole household to strictly quarantine right now. But, I also really dislike the feeling of trying to interact with people I know and love while wearing a mask. You miss so much of the experience of being with someone when you can't see their face or expressions. Instead of being uplifting to see them, it depresses me--and so I avoid those kinds of interactions as a protective coping mechanism. After all the depressing stuff I've been through this year, every little thing feels so much heavier than it should. I need to be putting together a lot more non-depressing experiences to rebuild my resilience. So (in cases where a mask is not required or specifically requested), I either say "no" to the get-together and avoid seeing anyone in person, or I say "oh forget it" and risk the interaction mask-free, which is wonderfully rejuvenating. But then I feel guilty or like I'm doing something "wrong" if I hug a friend or have a maskless meeting or get-together. I'm inconsistent at best, and I admit that. And I know I'm not alone in that constant back-and-forth struggle.
For me personally, I think it boils down to this: Sometimes, the risk of mental, emotional and social harm done by staying isolated is higher and more emergent than the risk of physically contracting or spreading COVID. So I guess that's my personal measuring stick. It's not perfect, and it's a sliding scale depending on the day and the circumstance and even the minute. Frankly, it's an exhausting decision-making process that happens multiple times a day, with every single request, event, outing, and interaction that we're faced with. I'm aware that sometimes how I behave may look careless or inconsistent from the outside looking in. But before you judge, please know that I'm doing the best I can to stay sane and survive--just like you are, just like everyone is in this insane world that we have to navigate.
So, that's the 5 week post-surgery, after cancer treatment, trying-to-put-my-life-back-together update. Clearly, I'm a work in progress in ALL the areas of my life. I guess that's nothing out of the ordinary for anyone...
Reconstruction: Air to Saline
This morning was the next step in my breast reconstruction after my mastectomies -- switching from air to saline in both tissue expanders.
The surgeon initially filled each tissue expander with air during surgery to give them shape, but keeping them lightweight while the incisions healed properly and fluid drained from around the expanders. Once the fluid had been drained sufficiently, the drains were removed (Monday) and then today (Friday), I went in to switch from air to saline.
To do that, they would deflate each side, and then inject the same amount of saline as air that was removed, which for me was 200cc on the left side and 150cc on the right. Which is a LOT of syringes of saline.
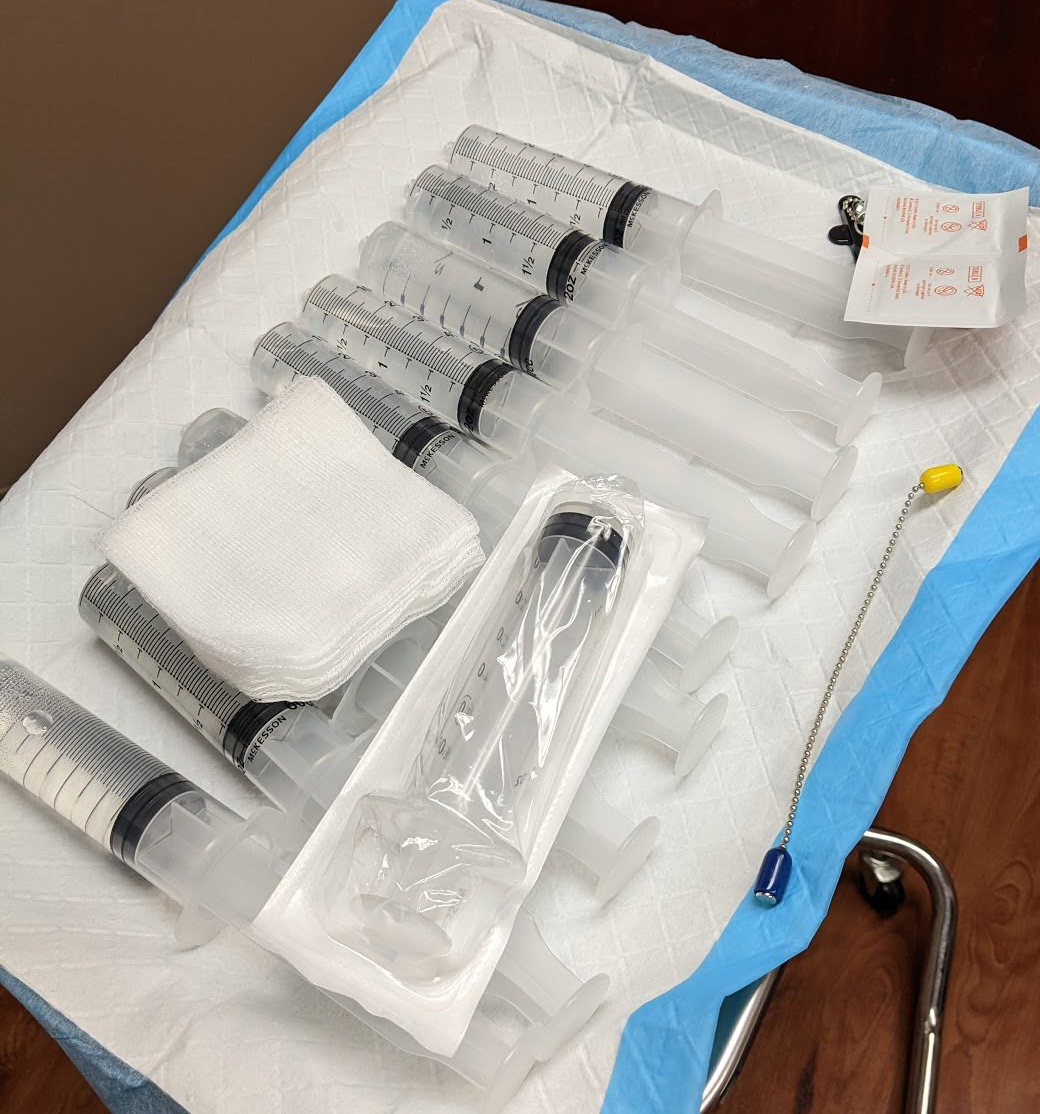
I was pretty nervous about this process. I knew after I'd done it once, I'd be ok to go back for fills on my own, but I asked Ben to come with me for this appointment. Turns out, I needed some hand-holding.
Here's a look at the type of expanders I have and how they work:
The nurse found the port for each expander with a little magnet, and then injected a giant butterfly needle to first remove the air with an empty syringe (I peeked, deflation was WAY weird) and then to insert the saline, 50ccs at a time. The needle hurt, but not any worse than having blood drawn, and just for a second. I couldn't really feel the deflating and saline injection at all though, so that was relieving. I did feel a little lightheaded and my stomach flipped a little bit, but I'm sure that was from nerves.
On the left side, where I've been way more bruised and had the drain in for two weeks longer than the other one, she also used the second port on the expander (explained in the video above) to remove some extra fluid from a seroma that had collected since the drain was removed earlier this week. That meant another big needle stick, but interestingly, that port was underneath one of the numb sections of my breast, so I didn't feel that one at all. Watching her remove that rusty-colored fluid into the syringe was pretty gross though--but after 4 weeks of draining fluid from my drains twice a day, it didn't bother me too much to see.
When it was all said and done, the expanders felt much better and softer and more "normal" with fluid inside them instead of air. They look a little rounder, which I imagine will continue to improve with each fill. And though I've been sore and tender throughout the day today, it was overall a pretty easy process--and more bizarre than anything else.
I'll have a couple more saline fills to get them to the right size over the next couple of weeks, but then the reconstruction process will be on hold for a few months while everything settles and continues to heal. I won't have my exchange to implants surgery until sometime this spring (likely).
It feels good to be moving forward.
Double Mastectomy: 4 Weeks Post Surgery
There's really very little to report about the past week (which was also Thanksgiving week) as far as progress or recovery.
I still had my left drain, which sloooowwly decreased in volume and turned more of a rusty dark brown from the dark maroon shade it had been. All the annoyances of having a drain continued throughout the week--sore drain site, poor mobility in my left arm, having to hook (and hide) a tube and bulb to my clothes, sleeping on my back with a wedge pillow, taking regular tylenol, ibuprophen, muscle relaxers and pain meds, etc.
The bruising and tenderness on my left side has subsided significanly (though not completely). The nerve pain and skin sensitivity continued through most of the week as well, although that has been less pronounced in the last couple of days. Unless I get the chills. Or yawn. Then ZING!
I kept my activity levels way down all week, per my breast surgeon's instructions hoping to keep that drain from producing any extra fluid. I spent most of everyday sitting or laying down, doing very little walking, and no lifting anything more than a couple of pounds.
We took a family trip to the beach for a few nights over Thanksgiving with Ben's parents, which is about a 4 hour drive from us. In full honesty -- I did NOT want to go. I was in a horrible mood leading up to the trip, physically uncomfortable, wasn't excited about dealing with a drain on the road and not in my own home, didn't want to make small talk, wasn't sure how to pack or what I'd be comfortable wearing, and was worried about the drive down being painful. But, I knew the kids and Ben needed the trip and the change of scenery might help me break out of my funk, at least a little bit. So I went -- but I'm sad to admit--not cheerfully. And I was definitely dead weight and completely unhelpful when it came to packing, preparing, planning, and parenting on this trip. Ben and his parents get ALL the credit for that!

While I did put my toes in the sand for a short period of time each day, I spent most of my time on the couch wrapped up in a blanket, and stayed medicated each evening to try and remain pleasant(ish) to be around.

Besides being physically uncomfortable, it was far too depressing for me to sit on the beach and see everyone around me in swimsuits getting tan and sandy, exercising and moving their bodies, when I was restricted to full-coverage bulky clothes, hiding a surgical drain and rock hard expanders and allowed little-to-no exercise. Many of my favorite beach activities were prohibited or awkward or uncomfortable. That (and the ever-presence of breasts in bikinis all around me) made it very difficult to temporarily forget my struggles.
I would say my mood was *slightly* lifted by the sand, the sun, a change in scenery and some holiday time with family. But boy was I in a rough spot when it took all of that to lift my spirits just a little bit. Yikes!
When we returned home, I was determined not to return to the dark dungeon of my bedroom recliner and Netflix and made myself get up, get dressed, and move around the house more over the weekend. Then, this morning at my appointment, my left drain was finally removed and I was (re)cleared to begin increasing my activity. Sweet relief!
My surgeons both said around 4 weeks most people "turn a corner" after the double mastectomy and expander reconstruction surgery I just had. Today marks 4 weeks, so I'm hoping that's true. Getting that last drain out will be a HUGE help in that, I'm sure.
Double Mastectomy: 3 Week Update
The past week had some ups and downs. After three days of walking for 25 to 35 minutes a day and beginning to push myself to become more active, that regimen was shut right back down by my breast surgeon on Wednesday, who said I was doing way too much. So, I spent the rest of the week sulking and sitting and doing more resting.
She was right, and I know it. But it sucks.
Having my right drain out since last Monday has definitely been an improvement. It allows me greater mobility with my right arm. I can reach above my head with that arm (to about 60 degrees before it starts to pull and hurt). I haven't had to worry about accidentally yanking on that drain tube, and the drain site incision has been slowly healing. It's still very tender to the touch, but is much better than having a tube coming out of it!
The left drain continues to be an annoyance, limits my arm mobility, and protecting it from getting pulled makes me hunch my shoulders forward way more than I should, which makes my back hurt. Unfortunately, it's still producing a decent amount of fluid and hasn't changed colors like it should, so it's sticking around until after Thanksgiving. That means I have another week to carry it with me.
Showering and getting dressed continues to be very difficult. Not impossible, and I'm able to do it myself, but I have to be very slow and methodical about it, and make sure I don't reach too far or pull on the drain tube. Generally, once I'm dressed, I'm in better shape, but the process of getting there is pretty exhausting and uncomfortable.
While my incisions are healing well, I'm still very bruised and tender across my entire chest and down my left side, so even the slightest touch can be painful and sensitive. Some people talk about their entire chest being numb after a mastectomy -- not the case for me. I have spots that are numb, but the rest of it is constantly tingling, burning, throbbing and extremely sensitive to touch or fabric, almost like the thin skin that is raw and sensitive after a burn. That seems to be getting more prominent, not less, and is probably the most uncomfortable and painful feeling so far. When it's constant, it's just so difficult to focus on anything else. Medications haven't seemed to help much to make it go away. Mindless distraction seems to be the best medicine for that ailment. I asked the nurse about it, and she said, unfortunately, it's common. I was afraid to ask if it's temporary or permanent...I'm not sure I want to know the answer. Maybe it means I will have feeling in most of my chest when this is all over, and it's ultimately a good thing.
I am still spending a lot of my time sitting in a recliner or laying in bed on my wedge pillow so that the pressure on my chest is slightly lessened. I want to wear the softest, stretchiest, most comfortable clothes I can find, because my skin is so extremely sensitive to anything that touches it. I'm still taking tylenol or ibuprophen a couple of times a day and a muscle relaxer and pain pill most evenings to release the tension and muscle tightness that has built up from protecting it all day long, and to help me fall asleep. Thankfully, I'm still sleeping well.
I usually have a couple hours of energy in the mornings (after two cups of coffee) where I can think pretty clearly, feel mostly ok, and am able to do something productive (but not physical). Sometimes that's a little bit of work, or catching up with emails or text messages, or reading or writing. Usually it's sitting at my desk or in the dining room or outside for some variety. But, by about 1pm, I'm fading fast, and spend the rest of the day in a recliner, on the couch or in bed.

I did start driving to run short errands in the middle of last week, and that has gone okay, but my limit is two stops on any outing, and nothing that takes very long to do. Parking lot spaces are a little hard for me to twist and turn and get out of safely. I went got my nails done on Friday, but being out for over an hour and sitting straight up in a chair was pretty taxing.
Mainly I'm waiting. Waiting for the drain to slow down so it can come out. Waiting for the bruising to go down so it hopefully doesn't hurt so badly. Waiting to be allowed to increase my activity. Waiting to switch from air-filled foobs to saline-filled foobs and see what kind of challenges that brings. Waiting to have enough mental and physical energy to go back to work. Waiting....
I had really hoped to be in better shape this week than I am. I'm still trying to stay the course and allow my body to heal properly, but it's been extremely tough mentally when I'm physically so uncomfortable. I kind of want to just sleep until I can wake up and feel better.
Honestly, I'm tired of hearing myself complain!
Ben has been a saint, taking care of EVERYTHING around the house and with the kids, and empathizing with all my sad sack whining. If he's complained about it, it hasn't been louder than me, so I couldn't hear it...
Hopefully by 4 weeks out, I'll have more progress to report.